Femia > Health Library > Getting Pregnant > Challenges > Best age to get pregnant with PCOS: When to start and what you need to know
Best age to get pregnant with PCOS: When to start and what you need to know

- Updated Feb 10, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
PCOS can impact fertility, but with proactive measures, lifestyle changes, and a tailored treatment plan, women with PCOS can significantly increase their chances of getting pregnant. Whether you’re in your 20s, 30s, or even beyond, it’s possible to conceive with PCOS. Interestingly, studies show that some women find the best age to get pregnant with PCOS is after 40, as they experience fewer symptoms and better management of the condition. Understanding how to get pregnant with PCOS involves considering factors like age, treatment options, and lifestyle adjustments.
Polycystic ovary syndrome (PCOS) is a common condition affecting women’s ovaries and reproductive health. One of the most common questions women with PCOS ask is, “How to get pregnant with PCOS?” While it may take longer and require more effort, getting pregnant with PCOS is definitely possible. Age is a significant factor in fertility, and it plays a role in how PCOS affects a woman’s ability to conceive. In this article, we’ll explore how women’s fertility changes over time, how to conceive with PCOS, and the best age to get pregnant with PCOS.
Femia offers the most accurate tool for determining ovulation and fertile days
PCOS explained: Causes and symptoms
Simply put, PCOS is a hormonal disorder that happens during the reproductive years. According to the National Library of Medicine, PCOS affects 4–18% of reproductive-aged women.
This disease causes small fluid sacs (called cysts) to develop along the outer edge of the ovary. These cysts contain immature eggs called follicles, which are unable to release eggs regularly.
PCOS is often difficult to diagnose or predict genetically since there is no exact cause of the disease known. However, statistics show that women who struggle with PCOS tend to have elevated levels of the luteinizing hormone and reduced levels of the follicle-stimulating hormone (FSH). And these imbalances may manifest as infrequent or lack of menstruation.
Although symptoms vary, women are usually diagnosed with PCOS when having at least two of these:
- Irregular periods: If having periods lasting for more than 7-9 days (a typical healthy period) or having fewer than nine periods a year, we recommend consulting a clinician because this is one of the main signs of PCOS.
- High androgen levels: Too much androgen is usually associated with excess facial and body hair, which is called hirsutism. Severe acne cases and male-pattern baldness may also be caused by high levels of androgen.
- Polycystic ovaries: Bigger ovaries are the result of many follicles containing immature eggs developing around the edge of the ovary.
(Note: PCOS symptoms are usually more severe in people struggling with obesity).
How does PCOS affect fertility?
PCOS is a common condition that can make it harder to get pregnant. It causes hormonal imbalances, leading to irregular periods and high levels of androgens (male hormones), which can disrupt ovulation. Without regular ovulation, it’s more difficult to conceive, making PCOS one of the leading causes of infertility.
👉Find out more: PCOS Belly: Why’s and how’s
@femia.fertility 🌟 Reminder for those who are trying to conceive 🌟 You are not alone. You are doing your best. There is nothing wrong with you. You are stronger than you thinkyou are. You deserve to have a baby and you will become a brilliant mother of one soon. We are here for you ❤️#mentalhealthawarenessmonth #infertilitywarriors #anxiety #mentalhealth #depression #infertility #ttccommunity #ttc #ttcsupport ♬ original sound - Femia fertility tracker
What is the best age to get pregnant with PCOS?
The best age to get pregnant with PCOS can vary for each woman, but fertility tends to be most optimal in your late 20s to early 30s. While PCOS can affect ovulation, many women still conceive naturally in this age range with the right lifestyle changes and medical support.
However, as you get older, particularly after the age of 35, fertility can decline, and it may take longer to conceive. The good news is that PCOS fertility can improve with age for some women, especially when paired with appropriate treatments such as medications to regulate ovulation. To increase your chances of getting pregnant with PCOS quickly, maintaining a healthy weight, reducing stress, and monitoring ovulation patterns are all important steps to take.
Fertility changes over years: Pregnancy with PCOS in your 20s, 30s, and 40s
While there is some evidence that PCOS symptoms may decrease with aging, the majority of experts still recommend to start trying to conceive sooner rather than later.
Here is how PCOS fertility changes throughout ages:
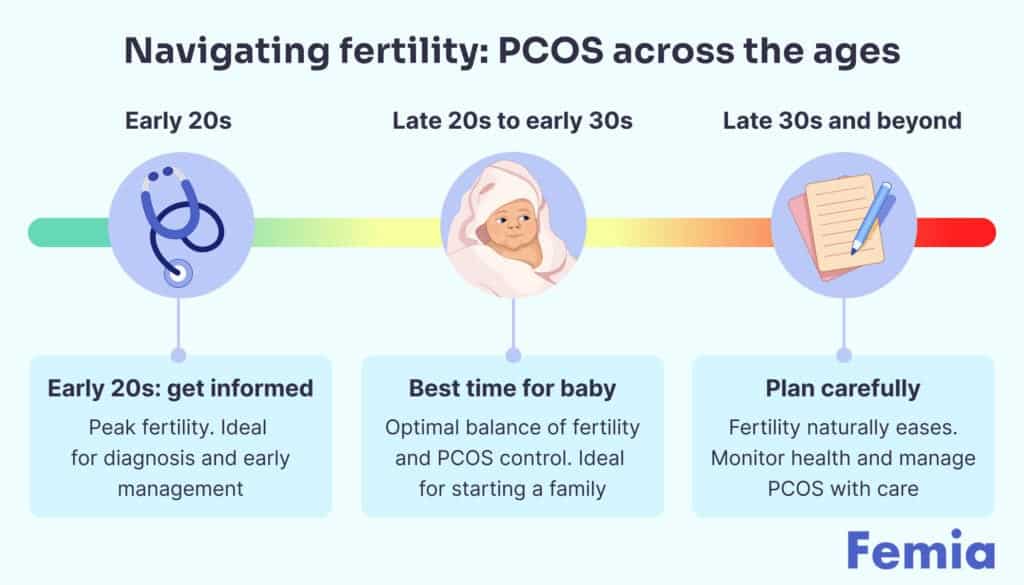
1. Early 20s with PCOS
Women in their early 20s have the highest fertility rates and a large ovarian reserve, even with PCOS. While fertility varies, consulting a physician is key to understanding your specific situation and options. PCOS is often diagnosed during this time, and taking proactive steps like lifestyle changes or egg freezing can help preserve fertility. Early action can increase your chances of getting pregnant with PCOS later in life.
2. Late 20s and early 30s — best age to get pregnant with PCOS
The best age to get pregnant with PCOS is often between 27-31. By this age, ovarian reserve remains high, and women typically have already started fertility treatments or made lifestyle changes to improve PCOS symptoms. This gives them a better chance of conceiving. While fertility begins to decline between 32-37, many women with PCOS can still get pregnant, though it may take longer.
3. The late 30s and further
Women with PCOS can still get pregnant after 35, but fertility declines more rapidly between 35-38. Age affects both the quantity and quality of eggs, and PCOS symptoms may lead to complications like miscarriage or birth defects. Although pregnancy is possible, it’s essential to discuss risks with a healthcare provider.
👉 Find out more: Boosting your fertility: Tips for getting pregnant in your 30s?
How to get pregnant with PCOS: Effective strategies
While there is no cure for PCOS, you can manage symptoms to reduce their effect on your ability to get pregnant. While in the majority of cases physicians prescribe drugs and treatment plans, there are several natural ways you can implement them without any harm.
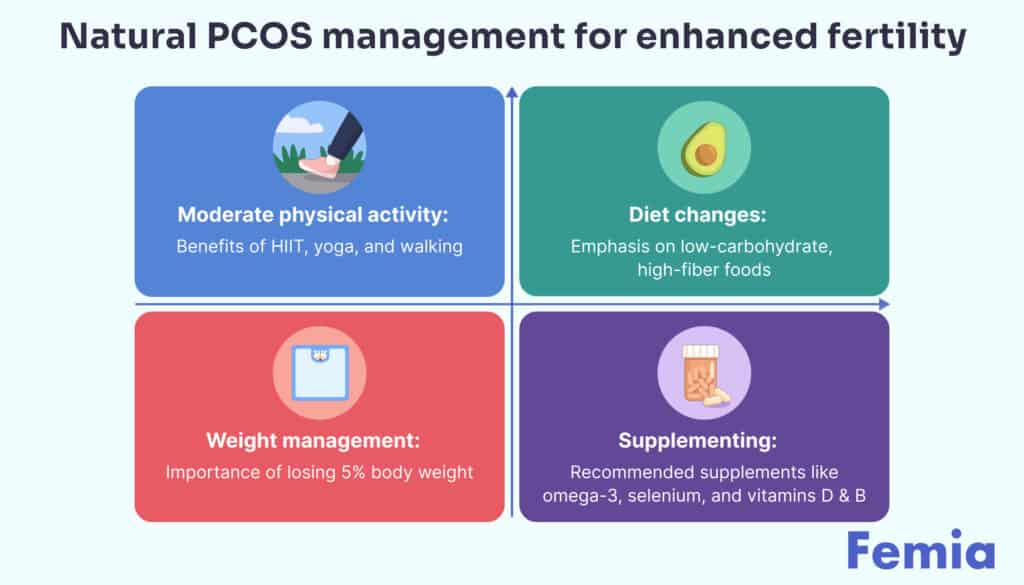
Moderate daily physical activity
Engaging in moderate daily physical activity is a key strategy in managing and reducing PCOS symptoms. Activities like walking for 30 minutes a day, high-intensity interval training (HIIT), yoga, or pilates have shown to have positive effects in managing insulin resistance and improving overall metabolic health. Regular physical activity helps regulate hormonal balance, improves insulin sensitivity, and can help with weight management, which is particularly important for women with PCOS. When asking “how to get pregnant with PCOS” or “how to ovulate with PCOS naturally,” regular exercise can significantly increase your chances by improving hormonal function and supporting ovulation.
Low-carbohydrate and high-fiber diet
Women with PCOS often struggle with insulin resistance, which is a common cause of fertility issues and other metabolic challenges. A low-carbohydrate, high-fiber diet helps reduce insulin levels and improve blood sugar regulation.
Focus on consuming complex carbs such as whole grains (like quinoa, brown rice, and whole wheat pasta), fruits, vegetables, and legumes. These foods have a low glycemic index, which helps stabilize blood sugar and can assist in conceiving with PCOS. Eliminate or limit foods with high glycemic indices, such as white bread, white rice, sugary cereals, cookies, sodas, and juices, as they can worsen insulin resistance and hinder fertility.
Weight management
Managing weight is crucial for women with PCOS, as insulin resistance can often lead to weight gain. Studies show that losing just 5% of body weight can significantly reduce the severity of PCOS symptoms, improve metabolic health, and increase fertility. Healthy weight loss is often a vital step in “how to get pregnant with PCOS quickly” as it helps regulate menstrual cycles and promotes ovulation. Even modest weight loss can result in significant improvements in hormonal balance, making it easier to conceive naturally.
Supplementing
Supplements like omega-3 fish oil, selenium, vitamin D, and vitamin B complex are commonly recommended for women with PCOS to help manage symptoms. According to a 2017 review, these supplements may support metabolic health, reduce inflammation, and improve fertility outcomes.
However, it’s important to remember that supplements should not replace medical treatment. Always consult your healthcare provider before starting supplements, as they may interfere with prescribed medications.

PCOS pregnancy success stories
There are anecdotal reports of women successfully managing PCOS symptoms through natural methods. 35-year-old Nia diagnosed with PCOS in her thirties, was able to naturally manage PCOS symptoms and dramatically improve life quality as well. She implemented several nutritional, supplemental, and lifestyle recommendations and had regular check-ins and guidance with a specialist.
Please note, that this is based on a private blog and cannot be considered a reliable source of information according to Femia standards. Always consult with your doctor for personalized advice and treatment options.
Diet changes, strength training, and doing pilates at home became a new norm that helped Nia:
- All lab markers returned to normal ranges (except for DHEA-S);
- Nia had had four consecutive 30-day cycles and ovulated three out of them (checked with regular ovulation testing);
- Periods were painless, with only mild discomfort on the first day;
- At the six-month mark, there were no signs of cystic nodules;
- She had regular bowel movements 1-2x per day with reduced sugar cravings;
- She lost eighteen pounds over the course of six months working with her specialist.
Exploring fertility treatments with PCOS
While managing PCOS symptoms naturally is possible and mostly used to improve life quality, getting pregnant with this disease usually involves the following fertility treatments:
1. Ovulation-inducing drugs
Depending on several factors, a healthcare professional may prescribe medications like clomiphene citrate (CC), letrozole, and metformin (an insulin sensitizer) as the first-line pharmacological treatment for anovulatory infertility (when not ovulating or releasing an egg).
Statistics show that about 78% and 95% of women diagnosed with PCOS will ovulate with CC and letrozole, respectively. Several studies described in the resource mentioned above also identified that letrozole live birth rates are higher than in women on CC ( 27.5% vs 19.1%)
👉 Find out more: Can you get pregnant when you’re not ovulating
Femia offers the most accurate tool for determining ovulation and fertile days
2. Second-line treatment
Gonadotropins are used as second-line agent treatments in PCOS-diagnosed women whose ovulatory functions did not improve with first-line oral ovulation medications (usually after 3-6 months without improvements). These are usually women resistant to oral drugs or those having undesirable antiestrogenic side effects.
Ovulation induction in this group of women tends to be more complex since it is hard to predict response to gonadotropin stimulation. If you are planning to use timed sex, this is why physicians include careful monitoring of the cycles with ultrasound and a strict cancellation policy of you have 2 follicles greater than 14mm
A study revealed a significantly higher clinical pregnancy rate, live birth rate, and cumulative pregnancy rate over three treatment cycles in patients with anovulatory PCOS for gonadotropins compared to clomiphene. The per cycle outcome was superior after ovulation induction with follicle-stimulating hormone compared to CC, with respect to the pregnancy rate per first cycle being 30% vs 14.6%.
3. Assisted reproductive technology
In Vitro Fertilization (IVF) is the third-line treatment and is usually considered in more complex cases, offering a higher pregnancy rate (reaching up to 50% from a single treatment cycle), especially in young women with high fertility levels and large ovarian reserve.
This treatment is commonly considered in case first- or second-line ovulation induction treatments were unsuccessful. Even offering high successful rates, IVF may come with significant challenges, including high risk of OHSS, multiple births, high cost, and variable access to treatment.
Questions from the Femia community
Does birth control impact future fertility for women with PCOS?
The short answer is no. Using birth control pills does not affect the ability to have a baby in the future. While hormonal birth control temporarily prevents pregnancy and delays fertility, required bodily functions will eventually get back to previous levels when you discontinue the contraceptive. In fact, birth control can be used as a treatment option for PCOS in women who want to reduce symptoms and consider getting pregnant later.
What precautions to take during pregnancy with PCOS?
Since high rates of miscarriage and gestational diabetes mellitus are related to increased insulin levels, pregnant women with PCOS should consider avoiding (or limiting) simple carbohydrates, like juices, soft drinks, sports drinks, candies, cookies, and other kinds of desserts.
What if I want to wait to have a baby?
First of all, always consult a doctor to decide on fertility treatment and get guidance on lifestyle changes. Aside from that, you may also want to consider freezing your eggs, adding moderate daily physical activity, improving the quality of your diet, and seeking support since both preparing and the pregnancy journey with PCOS could be emotionally hard.
Can I conceive naturally with PCOS?
Yes, it is possible to conceive naturally with PCOS. Many women with PCOS can get pregnant without medical intervention, especially if they manage their symptoms through lifestyle changes such as maintaining a healthy diet, exercising regularly, and managing weight. However, for some women, additional treatments like medication or fertility interventions may be needed to regulate ovulation and increase the chances of pregnancy. Always consult with a healthcare provider to discuss the best approach for your specific situation.
The bottom line
The journey to pregnancy for women with PCOS involves understanding and navigating reproductive challenges, but it is still possible to get pregnant with PCOS.
Experts suggest that the late 20s to early 30s is the best age to get pregnant with PCOS, with early and effective treatment management being crucial.
With several treatment options available, and considering the variation in each woman’s fertility rates and PCOS symptoms, it’s essential to seek personalized medical guidance to optimize fertility outcomes and answer the question, “How to get pregnant with PCOS?”
References
- Dennett, Carrie C., and Judy Simon. “The Role of Polycystic Ovary Syndrome in Reproductive and Metabolic Health: Overview and Approaches for Treatment.” Diabetes Spectrum, vol. 28, no. 2, May 2015, pp. 116–120. Diabetes Spectrum, https://doi.org/10.2337/diaspect.28.2.116.
- Cui, Yuqian, et al. “Age-specific Serum Antimüllerian Hormone Levels in Women with and without Polycystic Ovary Syndrome.” Fertility and Sterility, 18 Apr. 2014, https://doi.org/10.1016/j.fertnstert.2014.03.032.
- Pinola, Pekka, et al. “Androgen Profile through Life in Women with Polycystic Ovary Syndrome: A Nordic Multicenter Collaboration Study.” The Journal of Clinical Endocrinology & Metabolism, vol. 100, no. 9, 1 Sept. 2015, pp. 3400–3407. Oxford Academic, https://doi.org/10.1210/jc.2015-2123. Accessed 22 Apr. 2021.
- Wesselink, Amelia K., et al. “Age and Fecundability in a North American Preconception Cohort Study.” American Journal of Obstetrics and Gynecology, vol. 217, no. 6, 1 Dec. 2017, pp. 667.e1–667.e8. Elsevier, https://doi.org/10.1016/j.ajog.2017.09.002.
- Owen, Amy, and Paul B. Sparzak. “Age Related Fertility Decline.” StatPearls Publishing, 2022, www.ncbi.nlm.nih.gov/books/NBK576440/.
- Palomba, Stefano, et al. “Pregnancy Complications in Women with Polycystic Ovary Syndrome.” Human Reproduction Update, vol. 21, no. 5, 2015, pp. 575–592. PubMed, https://doi.org/10.1093/humupd/dmv029.
- Thakur, Deepshikha, et al. “Effect of Yoga on Polycystic Ovarian Syndrome: A Systematic Review.” Journal of Bodywork and Movement Therapies, vol. 27, July 2021, pp. 281–286. Elsevier, https://doi.org/10.1016/j.jbmt.2021.02.018.
- NIH. “Treatments to Relieve Symptoms of PCOS.” National Institute of Child Health and Human Development, 31 Jan. 2017, www.nichd.nih.gov/health/topics/pcos/conditioninfo/treatments/relieve.
- Arentz, Susan, et al. “Nutritional Supplements and Herbal Medicines for Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis.” BMC Complementary and Alternative Medicine, vol. 17, no. 1, 25 Nov. 2017, https://doi.org/10.1186/s12906-017-2011-x.
- Sawant, Shital, and Priya Bhide. “Fertility Treatment Options for Women with Polycystic Ovary Syndrome.” Clinical Medicine Insights: Reproductive Health, vol. 13, Jan. 2019, p. 117955811989086. PubMed, https://doi.org/10.1177/1179558119890867.

Bleeding during sex is a common complaint and is generally nothing to worry about. However, some cases require medical attention to treat the underlying cause.

Discover what happens at 26 weeks pregnant, from baby’s development and size to symptoms and self-care tips for a smooth journey.

How to stop your period: learn about your lifestyle and medical options that are safe and effective in shortening your period length.