Femia > Health Library > Getting Pregnant > Challenges > Female infertility: Causes, symptoms, and how to know if you’re infertile
Female infertility: Causes, symptoms, and how to know if you’re infertile
- Updated Feb 10, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
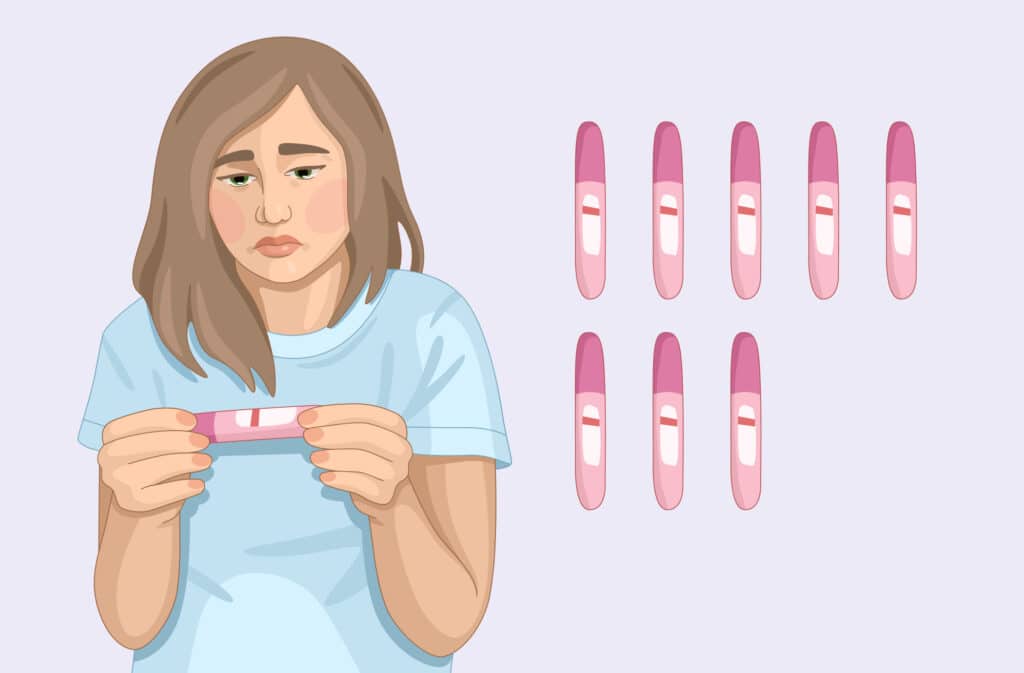
- Female infertility is defined as the inability to get pregnant after 12 months of regular unprotected sex.
- Common causes of infertility include hormonal imbalances, infections that affect the reproductive system (such as chlamydia or gonorrhea), structural issues like adhesions from previous surgeries or endometriosis, lifestyle factors, and age. These factors can disrupt normal reproductive function and are key contributors to difficulties in conceiving.
- Infertility treatment depends on the underlying cause but many women with infertility successfully conceive.
- Reaching out to your healthcare provider if you’re struggling to conceive is the crucial first step.
Female infertility is when women have difficulty conceiving under normal circumstances due to various factors.
We know that having infertility can be one of the most emotionally and physically challenging times for a woman and a couple. In this article, we are going to help you understand the topic, when to consult a doctor, and overview the treatment options.
What is female infertility?
According to the WHO, infertility will affect around one in six people during their lifetime and around 11% of women of reproductive age will suffer from infertility at some point in their lifetime. For a heterosexual couple experiencing infertility, female infertility accounts for the cause ⅓ of the time, male infertility ⅓ of the time, and both male and female infertility or unexplained infertility ⅓ of the time.
There are two types of female infertility:
- Primary infertility: This applies to women who have never been pregnant before.
- Secondary infertility: Refers to women who have previously achieved at least one clinical pregnancy, regardless of whether it resulted in a live birth, miscarriage, or stillbirth.
Understanding what type of infertility you have can help pinpoint a cause. Since treatment options and pregnancy success rates vary widely depending on the cause of infertility, this knowledge can be key to finding the right path forward.
When to see a healthcare provider for infertility
- You are under 35 and have been having regular unprotected sex for at least 12 months
- If you are over 35 and have been having regular unprotected sex for at least 6 months. This shortened timeframe is due to the natural decline in ovarian reserve that occurs with age, which can impact fertility.
If you have any concerns about your fertility, or you’re struggling to conceive, then reach out to your healthcare provider. They will be able to guide any fertility testing.
👉Find out more: Why am I not getting pregnant? Understanding common reasons for conception challenges
Signs and symptoms of infertility in women

The main sign of infertility in women is not being able to get pregnant despite having regular unprotected sex for a year. However, there can be some earlier warning signs that you might notice, these include:
- Irregular menstrual cycle: Cycles shorter than 21 days, longer than 35 days, or highly unpredictable may signal possible ovulation problems. However, irregular cycles do not always indicate infertility—some women with irregular cycles still ovulate and can conceive. Ovulation disorders can be associated with conditions such as polycystic ovary syndrome (PCOS), hyperprolactinemia, or thyroid dysfunction.
- Absent periods. The absence of periods, known as amenorrhea, may signal a lack of ovulation, which can prevent pregnancy. However, it can also result from other factors, such as issues with the hypothalamic-pituitary system, anorexia, hypothyroidism, or hyperprolactinemia. Primary amenorrhea refers to the absence of menstruation from adolescence, often linked to developmental or genetic conditions. Secondary amenorrhea occurs when menstruation stops during reproductive years, typically due to hormonal imbalances or chronic health issues. Both require medical evaluation to determine the underlying cause.
- Pain during sex. Experiencing discomfort or pain during sex can sometimes be a sign of underlying conditions like endometriosis or pelvic inflammatory disease. These conditions can impact female fertility due to chronic inflammatory processes that may lead to adhesions in the pelvic region, potentially affecting reproductive function.
- Chronic pelvic pain. Medical conditions like uterine fibroids, endometriosis, or pelvic inflammatory disease can cause long-term pain in your abdomen and may affect your fertility.
- Hormonal imbalances. Signs of a hormonal imbalance, such as excessive hair growth on the face or body, sudden weight changes, extreme fatigue, or acne, can indicate conditions like polycystic ovary syndrome (PCOS) or thyroid hormone issues. Both hypothyroidism and hyperthyroidism can disrupt ovulation by affecting the hypothalamic-pituitary-ovarian axis. Sudden weight changes, whether weight gain or loss, can also impact estrogen levels and ovulation, particularly in cases of severe weight loss or low body weight.
It can be difficult to know if you’re infertile without consulting a healthcare provider. While some women may have a medical condition or history that increases their risk of infertility, others may show no signs until they struggle to conceive after trying for a period of time.
Diagnosing infertility requires comprehensive evaluation, including tests for ovulation, a semen analysis for the partner, and an assessment of the fallopian tubes’ patency. However, in some cases, even after thorough investigation, the cause of infertility remains unknown—this is referred to as idiopathic infertility. Consulting a specialist is key to identifying potential issues and exploring treatment options.
What causes infertility in women?
There are several reasons for infertility in women, these can be physical, hormonal, age, and lifestyle-related. Here’s a look at some of the more common causes of female infertility:
| Cause | Description | Associated signs/symptoms |
|---|---|---|
| Hormonal disorders | Conditions like PCOS, thyroid imbalances, and hyperprolactinemia (high levels of prolactin) can disrupt ovulation and make conception harder. | • Irregular or absent periods
• Excessive hair growth • Sudden weight changes • Extreme fatigue For tips on how to get pregnant with PCOS we have put together a useful guide here. |
| Structural problems | Physical issues with your uterus or fallopian tubes can prevent pregnancy from happening. Blocked fallopian tubes, abnormal uterus shape, and fibroids can all prevent a sperm from reaching an egg or a fertilized egg from implanting in the uterus. | • Pain in abdomen
• Heavy periods • Inability to get pregnant • Irregular periods |
| Endometriosis | Estimated to affect 10–15% of reproductive-aged women, this inflammatory disease happens when the endometrium (lining of the uterus) grows outside of the uterus. | • Very painful periods
• Pain during sex • Heavy periods • Unable to get pregnant • Some women may have no symptoms For tips on how to get pregnant with endometriosis have a read of this helpful guide. |
| Infections | Certain sexually transmitted infections (STIs), like chlamydia or gonorrhea, can cause inflammation and scarring in the reproductive organs if left untreated. This results in pelvic inflammatory disease (PID) and can damage fallopian tubes leading to female infertility. | • Pain in the lower abdomen
• Pain during sex • Unusual vaginal discharge • Unpleasant smell from the vaginal region • Pain or difficulty urinating • Unusual bleeding between periods or after sex • Fever Some women will have no symptoms of having an STI or PID and won’t know until they struggle to get pregnant. |
| Early menopause | Also called “primary ovarian insufficiency” is when a woman’s ovaries stop working before she is 40. In about 90% of cases, the exact cause is unknown but it might be due to a genetic, metabolic, or autoimmune condition or linked to toxins or previous chemotherapy use. | • Irregular or missed periods
• Hot flashes • Night sweats • Anxiety • Irritability • Poor concentration • Reduced libido (sex drive) • Vaginal dryness • Pain during sex |
| Lifestyle factors | Obesity, smoking, excessive alcohol use, high stress levels, and exposure to certain chemicals can all impact your fertility. | • Irregular periods
• Absent periods • Symptoms of hormone imbalance |
| Age-related | Fertility naturally declines in your 30s, and by your 40s your chance of getting pregnant in any monthly cycle is around 5%. This is due to a natural decline in both the quantity and quality of your eggs. | • Shorter menstrual cycle
• Irregular periods • Unable to get pregnant For tips on how to get pregnant in your 30s and 40s have a look at these helpful guides. |
Unexplained infertility
In up to 25% of cases of infertility it’s not possible to identify the underlying cause. This can understandably be upsetting and frustrating, but not knowing the exact reason for your female infertility doesn’t mean that fertility treatment won’t work for you.
Top reasons for infertility when everything seems normal
Even when everything seems normal you can still experience infertility. Here are some common reasons why you might experience infertility:
- Egg quality decline. The quality of your eggs is just as crucial as the quantity. Even if you’re ovulating regularly and having normal periods, a higher proportion of abnormal eggs can significantly reduce your chances of conceiving. To assess ovarian reserve (the remaining quantity and quality of eggs), healthcare providers may recommend tests such as measuring anti-Müllerian hormone (AMH) levels and performing an ultrasound to evaluate the antral follicle count. These tests help determine your reproductive potential and guide appropriate treatment options.
- Mild endometriosis. Some women with mild endometriosis won’t have any symptoms, but this doesn’t mean the condition won’t affect fertility. It can be difficult to conceive when you have endometriosis, but for some women, it is still possible to naturally conceive with endometriosis. Treatment options, such as hormonal therapy or surgical intervention to remove endometrial lesions, can improve the chances of conception in many cases.
- Stress. High levels of stress can interfere with hormonal balance which can disrupt ovulation and affect fertility.
Can common factors cause infertility?
Some common factors can contribute to infertility, but there are many myths about female infertility, most of them lacking scientific support.
Myth: If you have PCOS you cannot get pregnant.
Truth: While PCOS is the most common cause of infertility, it doesn’t mean every woman with PCOS will be infertile. It is also one of the most treatable causes of infertility and many women with PCOS will have a successful pregnancy.
Myth: Taking birth control can cause infertility.
Truth: No, taking birth control doesn’t cause infertility. A 2018 meta-analysis of the evidence concluded that previous use of contraception, even for a long time, doesn’t significantly affect your fertility once you stop using it. On average, ovulation resumes within 1-3 months after discontinuing combined oral contraceptives (COCs). However, for long-acting injectable forms of contraception, it may take longer for ovulation and menstrual cycles to normalize. It’s important to discuss any concerns with your healthcare provider for personalized advice.
Myth: Female masturbation causes infertility
Truth: No, female masturbation doesn’t impact fertility. Guidelines from the Society for Reproductive Endocrinology and Infertility and the American Society for Reproductive Medicine, as outlined in their committee opinion doesn’t mention masturbation as a factor influencing fertility at all.
Diagnosis: How is female infertility evaluated?
In order to find out why you’re not getting pregnant you will need to be evaluated by a qualified healthcare professional. Some ways they might evaluate your fertility could include the following:
- Medical history and physical exam: Your doctor will likely begin with a detailed review of your medical and reproductive history, lifestyle factors, and any relevant health conditions. A physical exam, including a pelvic exam, might be performed to assess overall health and check for any visible signs of reproductive disease. Swabs of your vagina and cervix might be taken to look for infection or cervical disease.
- Hormonal testing: Blood tests are performed to assess levels of reproductive hormones that are critical for ovulation, such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Testing also includes thyroid hormones (TSH and free T4), as thyroid dysfunction—either hypothyroidism or hyperthyroidism—can significantly impact reproductive health. In addition, prolactin levels are checked since elevated prolactin can interfere with ovulation, and testosterone levels are evaluated if polycystic ovary syndrome (PCOS) is suspected. These tests provide a comprehensive understanding of hormonal factors that may affect fertility.
- Ovarian reserve testing: A blood test can evaluate your anti-Müllerian hormone (AMH) levels and an ultrasound can assess your follicles. Together these results can help predict the quantity and quality of your eggs.
- Imaging: A pelvic ultrasound can help check for abnormalities, such as ovarian cysts, fibroids, or structural issues in the uterus or ovaries that could impact fertility.
- Hysterosalpingography (HSG): This specialized X-ray procedure is used to check for blockages in the fallopian tubes by injecting a dye that flows through the tubes. If the dye doesn’t pass through, it may indicate a blockage, which can prevent the egg and sperm from meeting.
- Diagnostic surgery: Occasionally, your healthcare provider might recommend minimally invasive surgery where a small camera is inserted into your abdomen (laparoscopy) or uterus (hysteroscopy) to look for any visible signs of disease.
Treatment options for female infertility
After your fertility workup, your healthcare provider will have a clearer picture of what might be affecting your fertility and can suggest the best treatment options to help you move forward.
Treatment options can range from lifestyle adjustments to advanced medical procedures:
- Lifestyle changes. Sometimes, simple lifestyle adjustments can improve fertility. Maintaining a healthy weight, reducing stress, quitting smoking, limiting alcohol, and optimizing diet and exercise can all contribute to better reproductive health. Reducing alcohol consumption and quitting smoking are particularly important, as they not only benefit the woman but also significantly improve sperm quality in the male partner, further supporting conception efforts.
- Fertility medications. If the issue is around releasing an egg, then medications like Clomid (clomiphene citrate) can be prescribed to stimulate ovulation. Hormonal therapies may also be used to correct imbalances affecting ovulation, such as thyroid or prolactin issues.
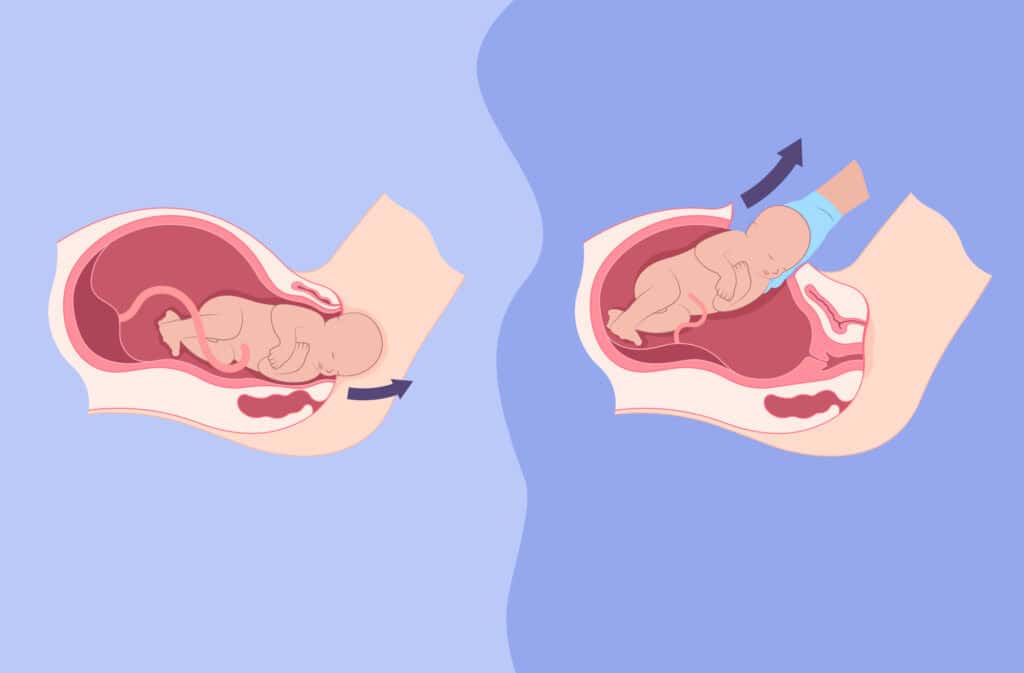
- Surgical options: If infertility is caused by structural issues such as fibroids, scarring from endometriosis or pelvic inflammatory disease (PID), or blocked fallopian tubes, surgery may be a viable treatment. Procedures can remove growths, scar tissue, or other obstructions that impact fertility. Laparoscopy is considered the “gold standard” for diagnosing and treating conditions like endometriosis, adhesions, or hydrosalpinx. This minimally invasive procedure allows for precise diagnosis and treatment, improving the chances of conception.
- Assisted reproductive technologies (ART). For some, ART is necessary to achieve pregnancy. The success of these technologies, such as in vitro fertilization (IVF), depends on various factors, including the cause of infertility, age, and ovarian reserve. Ovarian reserve is assessed through tests like anti-Müllerian hormone (AMH) levels and the antral follicle count, both of which are critical in predicting the likelihood of success with ART. Common ART procedures include:
- Intrauterine Insemination (IUI): Sperm is placed directly into the uterus around the time of ovulation, helping it reach the egg more easily.
- In Vitro Fertilization (IVF): The egg and sperm are combined outside the body in a lab to create an embryo, which is then transferred into the uterus.
These treatments can be tailored to each person’s situation. You often start with the simplest and least invasive methods and progress to more advanced options if needed.
👉Find out more: Can HPV cause infertility: Understanding the impact on fertility and pregnancy
Emotional support and coping strategies
Infertility can be extremely emotionally challenging. It is completely normal to feel stressed, angry, and wondering why infertility is happening to you. Finding coping strategies that work for you can make the journey feel a little easier and help you feel more supported. Here are a few potential strategies:
- Join a support group to connect you with other people also facing infertility to help you build a support network and feel less alone.
- Therapy with a therapist specializing in infertility can help you to process the complex emotions you might be feeling – like stress, anxiety, and grief.
- Open communication with your partner is key to helping you stay connected and feel understood. In times of difficulty this can be hard, so consider seeking couples counseling if you both feel you need some extra support.
Questions from the Femia community
Does stress really cause infertility?
Stress doesn’t directly cause infertility, but high stress levels can disrupt hormones and affect ovulation, potentially making it harder to conceive. It’s important to note though that while stress can play a role, it is rarely the sole cause of infertility.
Can infertility in women be reversed?
It depends on the cause; some conditions, like blocked tubes, hormonal imbalances or infertility caused by lifestyle factors, can be treated successfully and many women with infertility will go on to have successful pregnancies. Even if the infertility can’t be reversed, treatments like IUI and IVF can still result in a healthy pregnancy.
Is infertility permanent if you’ve had chlamydia?
Not always; early treatment of chlamydia can prevent there being any long-term damage at all, but untreated infections may lead to scarring and infertility.
Does exercising too much impact fertility?
Excessive exercise, particularly when combined with low body fat or insufficient caloric intake, can disrupt hormone levels and lead to irregular or absent menstrual cycles. This can affect fertility in some women but it is often reversible once exercise levels have reduced or a healthy BMI maintained.
Can fibroids cause infertility?
Fibroids, depending on their size and location, can interfere with implantation or block fallopian tubes, potentially causing infertility. If you have fibroids that are preventing you from getting pregnant, then surgery to remove them might restore your fertility.
The bottom line
Infertility is a common medical condition that affects many women worldwide. There are many different causes and identifying the underlying reason for infertility is a crucial first step. Hormonal imbalances, physical issues, lifestyle factors, pelvic infections, and age can all impact a woman’s ability to conceive.
Several different treatment options exist today— from lifestyle changes to assisted reproductive technologies— many women with infertility can go on to have successful pregnancies. If you have concerns about your fertility or are struggling to conceive, reach out to your healthcare provider. They can evaluate your unique situation and help determine the best path forward.
References
- “5 Lifestyle Choices That Can Affect Being Able to Get Pregnant.” Mayo Clinic, www.mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/female-fertility/art-20045887.
- “Abnormal Uterine Bleeding.” ACOG, www.acog.org/womens-health/faqs/abnormal-uterine-bleeding#:~:text=What%20is%20a%20normal%20menstrual,lasts%20up%20to%207%20days.
- ART Success Rates | CDC. www.cdc.gov/art/artdata/index.html.
- Author, Femia. “7 Steps to Getting Pregnant With Blocked Fallopian Tubes.” Femia Health, 17 Sept. 2024, femia.health/health-library/getting-pregnant/challenges/7-steps-to-getting-pregnant-with-blocked-fallopian-tubes.
- “Best Age to Get Pregnant With PCOS: Essential Tips – Femia.” Femia Health, 13 Sept. 2024, femia.health/health-library/getting-pregnant/challenges/best-age-to-get-pregnant-with-pcos.
- “Best Fertility Exercises: Workouts to Boost Conception Chances | Femia.” Femia Health, 17 Oct. 2024, femia.health/health-library/getting-pregnant/trying-to-conceive/fertility-exercises.
- “Boost Fertility: Tips for Getting Pregnant in Your 30s – Femia.” Femia Health, 13 Sept. 2024, femia.health/health-library/getting-pregnant/planning-pregnancy/tips-for-getting-pregnant-in-your-30s.
- “Enhancing Fertility Naturally: A Guide to Fertility Supplements and Foods for Women.” Femia Health, 8 Nov. 2024, femia.health/health-library/getting-pregnant/planning-pregnancy/fertility-supplements.
- “Fertility Diet: Best Foods to Boost Conception Chances | Femia.” Femia Health, 13 Sept. 2024, femia.health/health-library/getting-pregnant/trying-to-conceive/fertility-diet.
- “Getting Pregnant at 40: Navigating the Challenges and Opportunities.” Femia Health, 19 Sept. 2024, femia.health/health-library/getting-pregnant/challenges/getting-pregnant-at-40.
- “How to Get Pregnant With Endometriosis Naturally: Tips and Strategies.” Femia Health, 13 Sept. 2024, femia.health/health-library/getting-pregnant/challenges/how-to-get-pregnant-with-endometriosis.
- “How to Improve Egg Quality: 9 Tips for Better Fertility | Femia.” Femia Health, 13 Sept. 2024, femia.health/health-library/getting-pregnant/challenges/how-to-improve-egg-quality.
- “How to Increase Fertility in Women: 7 Natural Ways | Femia.” Femia Health, 13 Sept. 2024, femia.health/health-library/getting-pregnant/trying-to-conceive/how-to-increase-fertility-in-women.
- Department of Health. “Age And Fertility.” Better Health Channel, www.betterhealth.vic.gov.au/health/conditionsandtreatments/age-and-fertility.
- “Endometriosis – Symptoms and Causes.” Mayo Clinic, www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656.
- Girum, Tadele, and Abebaw Wasie. “Return of Fertility After Discontinuation of Contraception: A Systematic Review and Meta-analysis.” Contraception and Reproductive Medicine, vol. 3, no. 1, May 2018, https://doi.org/10.1186/s40834-018-0064-y.
- “How Common Is Infertility?” https://www.nichd.nih.gov/, 8 Feb. 2018, www.nichd.nih.gov/health/topics/infertility/conditioninfo/common.
- “Hypothyroidism (Underactive Thyroid) – Symptoms and Causes.” Mayo Clinic, www.mayoclinic.org/diseases-conditions/hypothyroidism/symptoms-causes/syc-20350284.
- Macer, Matthew Latham, and Hugh S. Taylor. “Endometriosis and Infertility.” Obstetrics and Gynecology Clinics of North America, vol. 39, no. 4, Nov. 2012, pp. 535–49. https://doi.org/10.1016/j.ogc.2012.10.002.
- National Library of Medicine. “Primary Ovarian Insufficiency.” POI | MedlinePlus, medlineplus.gov/primaryovarianinsufficiency.html#:~:text=Primary%20ovarian%20insufficiency%20(POI)%2C,as%20they%20transition%20to%20menopause.
- “Optimizing Natural Fertility: A Committee Opinion.” Fertility and Sterility, vol. 117, no. 1, Nov. 2021, pp. 53–63. https://doi.org/10.1016/j.fertnstert.2021.10.007.
- “Pelvic Inflammatory Disease (PID) – Symptoms and Causes – Mayo Clinic.” Mayo Clinic, 30 Apr. 2022, www.mayoclinic.org/diseases-conditions/pelvic-inflammatory-disease/symptoms-causes/syc-20352594.
- “Polycystic Ovary Syndrome | Office on Women’s Health.” OASH | Office on Women’s Health, www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome#:~:text=Having%20PCOS%20does%20not%20mean,you%20can’t%20get%20pregnant.
- “Polycystic Ovary Syndrome (PCOS) – Symptoms and Causes.” Mayo Clinic, www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439.
- Website, Nhs. “Infertility.” nhs.uk, 11 Aug. 2023, www.nhs.uk/conditions/infertility.
- World Health Organization: WHO. “1 in 6 people globally affected by infertility: WHO.” World Health Organization, 4 Apr. 2023, www.who.int/news/item/04-04-2023-1-in-6-people-globally-affected-by-infertility#:~:text=Around%2017.5%25%20of%20the%20adult,care%20for%20those%20in%20need.
- Infertility. 22 May 2024, www.who.int/news-room/fact-sheets/detail/infertility#:~:text=Primary%20infertility%20is%20when%20a,diagnosis%20and%20treatment%20of%20infertility.
- Sexually Transmitted Infections (STIs). 21 May 2024, www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis).
- World Health Organization: WHO and World Health Organization: WHO. Polycystic Ovary Syndrome. 28 June 2023, www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome.

What is ureaplasma? Discover the symptoms of Ureaplasma in females, how it is diagnosed, and the treatments. Learn how this infection can impact fertility and well-being.
Explore the differences between C-sections and vaginal births including risks recovery time and what factors you should consider before making a choice.
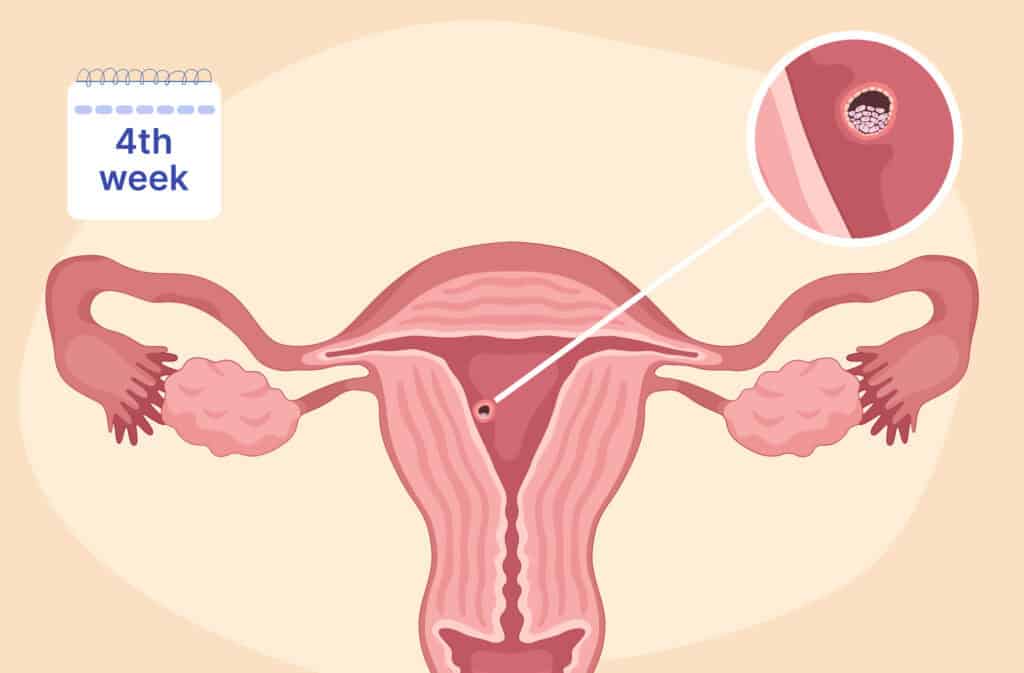
Learn about week 4 pregnancy symptoms, baby size, and the changes happening in your body as you progress in early pregnancy.

