Femia > Health Library > Getting Pregnant > Challenges > Male Infertility: Causes, symptoms, and what you need to know
Male Infertility: Causes, symptoms, and what you need to know
- Updated Feb 10, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
Male infertility contributes to half of infertility cases globally. The most common causes include low sperm count, decline in sperm quality, hormonal disorders, obstruction to sperm release, and lifestyle factors.
Observing pain, difficulty maintaining an erection, or an inability to conceive after trying are possible signs of male infertility. Simple lifestyle changes can help to improve male infertility symptoms. Medical treatment may include medications such as anastrozole or clomiphene citrate, depending on hormonal imbalances, such as low testosterone levels related to high estrogen. In some cases, simple surgical procedures may be used based on the underlying cause of male infertility.
Male infertility is the male factor contributing to infertility. Globally, 8–12% of couples struggle with infertility, and male factor infertility contributes to 50% of these cases. The primary cause can often be traced back to the male reproductive system. Low sperm count or quality, obstruction in the vas deferens, and medical conditions such as varicoceles and erectile dysfunction are among the common causes of male infertility.
A man’s lifestyle also contributes, and small improvements in lifestyle can frequently improve underlying causes of male infertility. If you and your partner have been trying to get pregnant for over a year, follow through the article to find out if male factor infertility may be a cause and what possible options in treatment might be available.
What is male factor infertility?
Most couples, about 90%, conceive within their first year of trying. An inability to conceive after 12 months of trying is referred to as infertility. For couples where the woman is over 35 years old, the timeframe for diagnosing infertility may be reduced to 6 months. Male factor infertility refers to a male factor contributing to the inability to conceive naturally after one year of regular unprotected intercourse. This can involve issues with sperm quality, quantity, or motility.
Since healthy sperm plays a crucial role in fertilizing an egg, this is considered the primary cause of male factor infertility. One of the first things checked when you visit a fertility expert is sperm quantity, quality, and delivery. Most causes of infertility, both internally and externally, affect either sperm production or its delivery to meet the egg.
What causes male infertility?
As we have just highlighted, the primary cause of male factor infertility is related to sperm. So, the first cause linked with infertility in men would be in the production and quality of sperm. Following this, obstructive causes, such as those hindering the delivery of sperm, will be sought out.
What are the 4 causes of male infertility?
1. Sperm quality and quantity
About 40–50% of male factor infertility is due to oligospermia or azoospermia, which is the reduction or complete absence of sperm. The normal average number of sperm per ml of semen is typically considered to be at least 15 million sperm, according to some standards. However, according to the fifth edition of the World Health Organization’s (WHO) “Laboratory Manual for the Examination and Processing of Human Semen” (2010), a sperm sample is considered normal if at least 4% of sperm have normal morphology. This threshold is based on studies of men whose partners became pregnant within the last 12 months. After sperm quantity, sperm quality is also assessed, which includes factors like morphology and motility.
2. Medical conditions
Varicoceles are dilated veins in the scrotum. These can affect the production and pathway of sperm. If the quality of the sperm production is affected, even if produced in sufficient numbers, they might not be able to reach and fertilize the egg.
Infections and inflammatory conditions, such as epididymitis or prostatitis, can also affect the quality and motility of sperm produced. It is reassuring to know that treating these underlying conditions slowly improves both sperm quality and quantity.
3. Hormonal disorders
Hormonal disorders are those impacting testosterone production. This can either be in the pituitary or through limitations within the reproductive glands. During a male infertility check-up, your testosterone levels will be evaluated—a crucial hormone favoring the production and release of sperm.
4. Erectile and ejaculatory conditions
Erectile dysfunction can result from many related causes. Some can be psychological, while others are physical, such as taking a new medication, the presence of scar tissue, or underlying health conditions, such as diabetes. Ejaculation is also assessed during male infertility tests, observing whether there is premature or retrograde ejaculation, which prevents sperm from reaching the egg.
5. Other causes
Rarely, underlying genetic disorders may contribute to infertility in men. Some of these syndromes include Robertsonian translocation, cystic fibrosis, and Klinefelter syndrome.
While Klinefelter syndrome is relatively rare, it should be tested for, especially in cases of unexplained azoospermia, where no sperm is found in the semen. Identifying genetic causes is important for determining the appropriate treatment options and understanding the chances of conception.
👉Find out more: Genetic testing before pregnancy: Importance, types and benefits for conception
Can drugs cause infertility in men?
Certain medications and recreational drugs can impact both sperm quality and quantity.
1. Anabolic steroids
These provide an external supply of hormones, reducing the natural production of testosterone. Anabolic steroids limit both the quantity and quality of sperm produced, causing male infertility. There is also possible destruction of sperm-producing cells if anabolic steroids are used for longer durations.
2. Medical drugs
Medicines used to treat high blood pressure, indigestion, and even depression can either affect sperm or cause erectile dysfunction, resulting in male infertility symptoms. Before you start any of these medications, it is crucial to inform your doctor if you and your partner are trying to conceive. In addition, chemotherapy drugs, used to treat cancer, can damage both sperm and sperm-producing cells. For men undergoing cancer treatment, it’s advisable to consider sperm banking before starting chemotherapy, as it can affect fertility and may cause long-term damage to sperm production.
3. Recreational drugs
Preliminary studies have shown that street drugs such as marijuana, cocaine, and opiates have the potential to affect sperm production and quality. The extent of the damage is still vastly unknown, but refraining from its use has numerous benefits, especially when trying to get pregnant.
How to know if you’re an infertile male?
When you and your partner have been trying to conceive for a minimum of 12 months, the inability to do so is an indication of infertility. Along with tests for female causes of infertility, signs of male infertility will be evaluated during a preliminary check-up with a fertility specialist.
Signs of male infertility
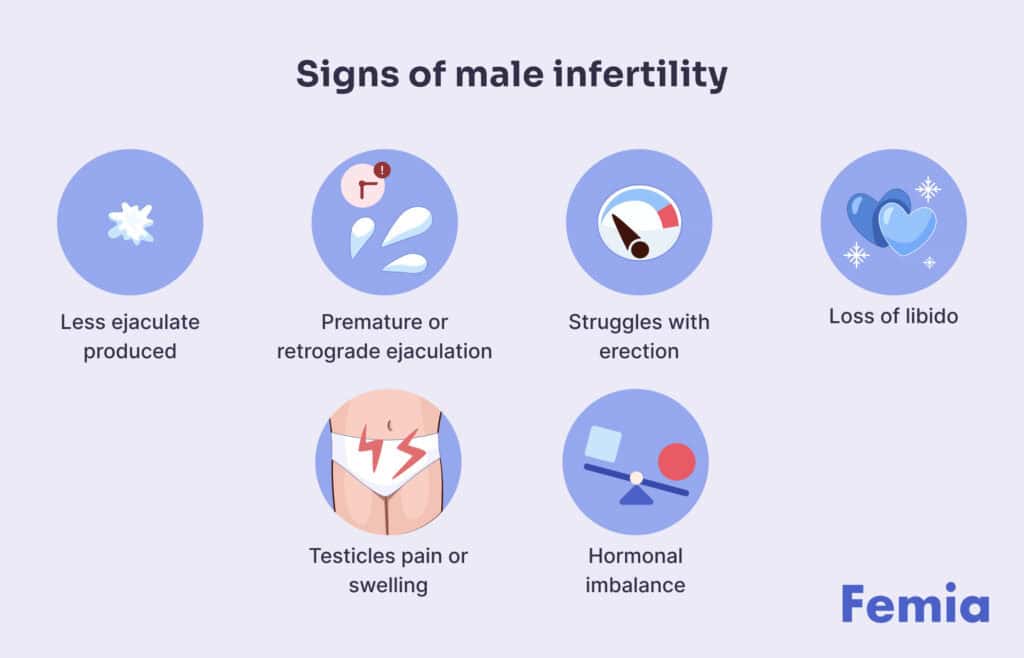
Sometimes it may not require a whole year of trying to notice a possible clue of male factor infertility. Male infertility symptoms might present earlier and can include:
- Less ejaculate produced
- Premature or retrograde ejaculation
- Struggles with maintaining an erection
- Loss of your normal libido
- Swelling or pain in and around the testicles
- Signs of hormonal imbalance (breast growth, reduced facial/body hair)
Noticing any or a combination of these signs of male infertility should prompt a visit with your healthcare provider.
Diagnostic tests for male infertility symptoms
Initially, your doctor will take a comprehensive medical history to understand both physical and lifestyle causes that could be contributing to male infertility. Medical history may also prompt the diagnosis of underlying genetic conditions that may have been overlooked.
Some of the initial diagnostic tests your doctor may consider include:
- Semen analysis to check for sperm count, motility, and morphology
- A full blood test, also checking for hormone levels
- A scrotal and transrectal ultrasound, which can help detect conditions such as a varicocele and other obstructions in the path semen takes
- If medical history indicates, a genetic analysis
In some cases, a testicular biopsy or specialized semen function tests may also be considered
At what age do men become infertile?
In conjunction with declining sperm counts, sperm quality also shows a noticeable decline with age. The accumulation of DNA damage within sperm through increased DNA fragmentation increases with age, resulting in higher levels of oxidative stress, lowering sperm quality.
Is male infertility permanent?
You’ll be reassured in knowing that most cases of male infertility symptoms are treatable. Having a medical condition such as varicocele can be managed through a simple outpatient medical procedure.
Additionally, conditions such as infection or inflammation can be managed with medications. Blockages of the vas deferens, or even if you’ve had a vasectomy, can be reversed with a simple procedure that requires only a short recovery period.
Most of the cases we have observed above, which result in a decline in the quantity and quality of sperm, can also be managed through simple lifestyle changes. The natural decline in sperm counts with age, or genetic disorders contributing to sperm abnormalities, unfortunately may not be reversible.
Treatment options for male infertility
After you have consulted with your fertility expert, the first step usually recommended is a lifestyle change. Additionally, based on your symptoms, there are medical and surgical options your healthcare provider will discuss with you.
👉Find out more: My husband takes testosterone injections. Can I still get pregnant?
Medical treatment options
If, during your examination, your hormone levels are observed to be low, medications such as clomiphene citrate or aromatase inhibitors (e.g., anastrozole) may be recommended to address hormonal imbalances and improve sperm count and quality. Testosterone supplements are not used to stimulate spermatogenesis, as there is evidence suggesting they may actually suppress it.
The American Society for Reproductive Medicine (ASRM) emphasizes that treatments for male infertility due to hormonal imbalance should focus on medications that stimulate the natural hormonal cycle, rather than using exogenous testosterone. Studies published in journals like Fertility and Sterility confirm that aromatase inhibitors and clomiphene citrate are effective in improving sperm quality in men with low testosterone levels.
Surgical treatment
Surgery is often used to manage blockages, such as those noted with scarring from previous injury or infection. Additionally, surgery can also be used to treat varicoceles or for vasectomy reversals.
Assisted Reproductive Technology
After attempts have been made with lifestyle changes and other medical management for male infertility, assisted reproductive technology (ART) is explored. Procedures such as intrauterine insemination (IUI) or in vitro fertilization (IVF), make use of viable sperm. With IUI, the sperm is directly placed into the uterus around ovulation, increasing chances of fertilization. With IVF, eggs are fertilized with sperm externally, then implanted into the uterus.
👉Find out more: Female infertility: Causes, symptoms, and how to know if you’re infertile
Lifestyle changes to improve infertility in men
Often, with male infertility, simple lifestyle changes are sufficient to improve sperm quantity and quality. These can also help to boost testosterone levels naturally, crucial for encouraging sperm production.
Maintain a healthy weight and balanced diet
A review of literature has reported that significant weight loss, especially for men who are obese, drastically improves sperm quantity, morphology, and testosterone levels. A combination of diet and exercise-induced weight loss has also been shown to decrease sperm DNA fragmentation. Sperm-boosting foods, including those rich in omega-3 fatty acids, antioxidants, vitamins, and essential minerals, such as zinc and selenium, lower the risk of male infertility.
Avoid excess heat exposure to your testicles
Heat exposure from saunas, hot baths, tight underwear, and even high fevers can affect sperm production. Additionally, excessive use of laptops placed on laps can also increase scrotal temperature, potentially impacting sperm quality and fertility. While most causes are reversible, prolonged and repeated exposure can also affect sperm motility. This correlation between increased heat exposure and changes in sperm production was higher in men > 30 years of age.
Cut down on alcohol and smoking
Excessive smoking was linked with lowering sperm count, while chronic alcohol use resulted in morphologically abnormal sperm, in a study conducted on 62 healthy men. Short-term use frequently results in reversible changes, with improvements seen almost instantly. It is still possible to get pregnant with initial changes in sperm morphology; however, ridding yourself of these habits can lead to benefits beyond just an improvement in fertility.
Manage your daily stressors
It has been clinically shown that testicular function and sperm quality are impacted by psychological stress. These stressors can come from relationships, finances, or even the stress of conceiving. While stress is often subjective, it becomes crucial when treating male infertility. Taking time to relax, creating a more structured routine, and delegating tedious tasks can help alleviate some odalisque stress.
Questions from the Femia community
Can male infertility be genetic?
Yes, in some instances, it can be. Having genetic conditions such as cystic fibrosis, Klinefelter syndrome, or chromosomal translocations or microdeletions can result in a decline in sperm production and their quality, affecting fertility.
Does frequent ejaculation reduce fertility?
Sperms are produced in the millions daily. So, frequent ejaculations will not reduce the quantity of sperm. However, for more effective sperm levels per ejaculate, especially if you are trying to get pregnant, spacing out penetrative intercourse every 1–2 days is optimum.
Can infections such as Chlamydia cause male infertility?
Yes, infections contribute to infertility in men, especially if untreated. Having previous or recurrent infections, or not getting your infections promptly managed, can result in inflammation and scarring of the reproductive tract. This can limit the effective transportation of sperm, lowering the chances of getting pregnant.
The bottom line
Male factor infertility contributes to approximately 50% of issues that couples face when trying to conceive. The primary causes include sperm quantity and quality, hormonal imbalances, and possibly obstructive causes. Since infertility in men is multifactorial, with lifestyle, age, and underlying medical conditions contributing, management requires an individualized approach.
Male infertility is often diagnosed during a fertility check-up. Evident male infertility symptoms might be present if there is an underlying cause such as an infection or varicocele. Most cases are treatable, either with alterations in lifestyle, medical management, or small surgical procedures. If these don’t help improve the chances of pregnancy, alternatives, such as assisted reproductive technology, can be explored.
References
- Agarwal, Ashok, et al. “Male Infertility.” The Lancet, vol. 397, no. 10271, Dec. 2020, pp. 319–33. https://doi.org/10.1016/s0140-6736(20)32667-2.
- Taylor, A. “Extent of the Problem.” BMJ, vol. 327, no. 7412, Aug. 2003, pp. 434–36. https://doi.org/10.1136/bmj.327.7412.434.
- Plaseska-Karanfilska, Dijana, et al. “Genetic Causes of Male Infertility.” Balkan Journal of Medical Genetics, vol. 15, no. Supplement, Dec. 2012, pp. 31–34. https://doi.org/10.2478/v10034-012-0015-x.
- Osta, Rabih El, et al. “Anabolic Steroids Abuse and Male Infertility.” Basic and Clinical Andrology, vol. 26, no. 1, Feb. 2016, https://doi.org/10.1186/s12610-016-0029-4.
- Dohle, Gert R. “Male Infertility in Cancer Patients: Review of the Literature.” International Journal of Urology, vol. 17, no. 4, Feb. 2010, pp. 327–31. https://doi.org/10.1111/j.1442-2042.2010.02484.x.
- Schifano, Nicolò, et al. “Recreational Drug Misuse and Its Potential Contribution to Male Fertility Levels’ Decline: A Narrative Review.” Brain Sciences, vol. 12, no. 11, Nov. 2022, p. 1582. https://doi.org/10.3390/brainsci12111582.
- Da Silva, Sarah Martins, and Richard A. Anderson. “Reproductive Axis Ageing and Fertility in Men.” Reviews in Endocrine and Metabolic Disorders, vol. 23, no. 6, Nov. 2022, pp. 1109–21. https://doi.org/10.1007/s11154-022-09759-0.
- Johnson, Larry, et al. “Quantification of the Human Sertoli Cell Population: Its Distribution, Relation to Germ Cell Numbers, and Age-Related Decline 1.” Biology of Reproduction, vol. 31, no. 4, Nov. 1984, pp. 785–95. https://doi.org/10.1095/biolreprod31.4.785.
- Vaughan, D. A., et al. “DNA Fragmentation of Sperm: A Radical Examination of the Contribution of Oxidative Stress and Age in 16 945 Semen Samples.” Human Reproduction, vol. 35, no. 10, June 2020, pp. 2188–96. https://doi.org/10.1093/humrep/deaa159.
- Ameratunga, Devini, et al. “Obesity and Male Infertility.” Best Practice & Research Clinical Obstetrics & Gynaecology, vol. 90, Aug. 2023, p. 102393. https://doi.org/10.1016/j.bpobgyn.2023.102393.
- McKinnon, Craig J., et al. “Male Personal Heat Exposures and Fecundability: A Preconception Cohort Study.” Andrology, vol. 10, no. 8, Aug. 2022, pp. 1511–21. https://doi.org/10.1111/andr.13242.

Did you know your clitoris can be the key to unlocking your orgasm? Follow this guide for enhancing your clitoral satisfaction, and maximizing your sexual experience.

Discover safe and comfortable sex positions during pregnancy that enhance intimacy while accommodating bodily changes. Explore positions that prioritize comfort and intimacy, ensuring both partners feel connected and at ease.

Learn how to distinguish implantation bleeding from your period. Discover key differences in timing, flow, and symptoms. Expert advice from Femia on early pregnancy signs.

