Femia > Health Library > Getting Pregnant > Planning pregnancy > How do I know if I am fertile enough to get pregnant? Key signs and tips
How do I know if I am fertile enough to get pregnant? Key signs and tips

- Updated Feb 11, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
Fertility signs include regular menstrual cycles, cervical mucus changes, a slight rise in basal body temperature, and possible ovulation pain. Monitoring ovulation through kits, hormonal tests, ultrasounds, and ovarian reserve testing can help assess fertility. Reach out to your healthcare provider for personalized advice.
When trying to conceive, understanding your fertile window is key. This period, typically a few days before and during ovulation, offers the highest chance of pregnancy. Fertility signs like changes in cervical mucus, a slight increase in body temperature, and ovulation pain help you pinpoint this window. By paying attention to your body’s signals and using tools like ovulation tests, you can optimize your chances of getting pregnant. Even if you’ve never thought much about the way the female body works, now is the time to learn.
Understanding fertility and the menstrual cycle
Everybody seems to be talking about the treatment of infertility, but how much do you know about fertility itself? Infertility is a medical condition diagnosed when a woman is unable to get pregnant. Fertility, the opposite term, refers to your natural ability to conceive and bear children.
Many factors can influence a woman’s fertility. Having regular menstrual cycles, during which an egg is released from the ovaries (ovulation), is a prerequisite for conception. A healthy reproductive tract—including the fallopian tubes (tubes that connect the ovaries to the uterus), uterus, and cervix—is essential for the sperm to meet the egg and fertilize it.
Certain times of the month are associated with high and peak fertility. This is because of your menstrual cycle—the monthly process guided by sex hormones—which consists of four phases:
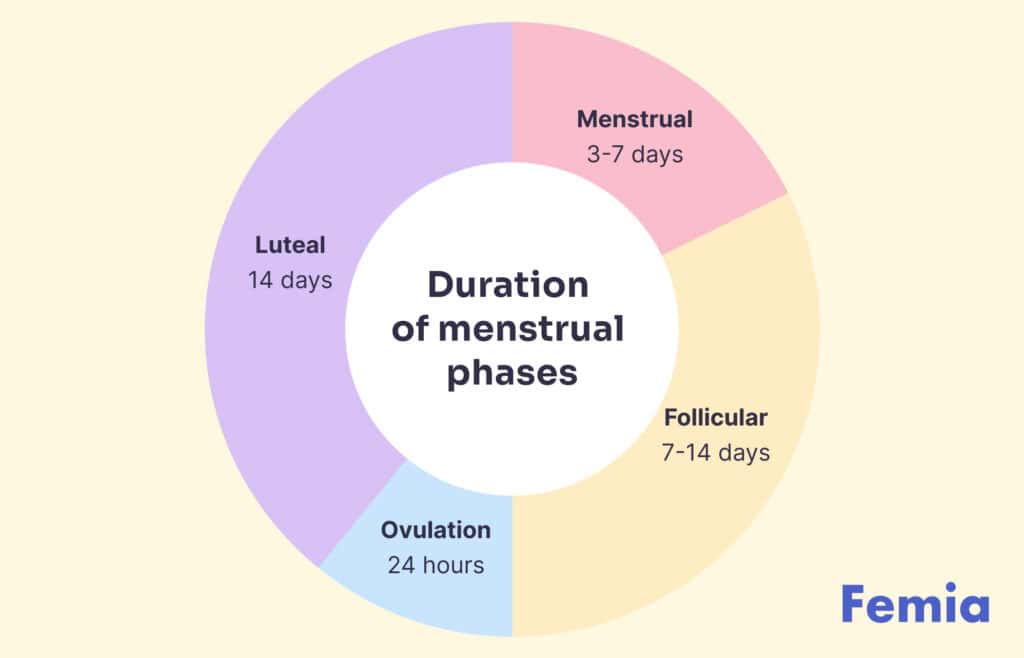
- Follicular phase. Estrogen and follicular stimulating hormone (FSH) levels start to increase. Follicles in your ovaries grow, while the uterus lining thickens.
- Ovulation. An increase in luteinizing hormone (LH) level makes an egg pop from the follicle, which causes bloating—a process also known as ovulation. Estrogen levels also peak around this time, before dropping until the next cycle.
- Luteal phase: After ovulation, the popped follicle transforms into a structure called the corpus luteum, which produces progesterone. Progesterone helps thicken the uterine lining further, in case a fertilized egg gets implanted. If this doesn’t happen, progesterone levels decrease.
- Menses phase: This is the time of menstrual bleeding, which marks the beginning of a new cycle. Low levels of both estrogen and progesterone signal the body to start shedding the uterine lining.
The time of the month when you are most likely to get pregnant (high and peak fertility) is also known as the ”fertility window.“ For most women, the fertility window starts about five days before ovulation and lasts until the day after. If you are trying to conceive, the fertility window will be the best time to have sex.
What is the fertile window?
The fertile window refers to the period in your menstrual cycle when you are most likely to conceive. It typically lasts about 6 days—5 days before ovulation and the day of ovulation itself. This is because sperm can survive in the female reproductive tract for up to five days, but an egg only lives for about 24 hours after ovulation. Understanding your ovulation window can help you time intercourse for the highest chance of pregnancy. Tracking changes in cervical mucus, basal body temperature, or using ovulation predictor kits can help identify this critical window.
The best time to get pregnant in the fertile window
How do I know if I am fertile enough to get pregnant?
Physical signs of fertility
How do you know if your fertility is high? Well, there will be signs your body is ready for pregnancy.
- Your menstrual cycles are regular. Whether your menstrual cycle is 26 or 32 days long (both are okay!), consistency is what matters. Your period coming at the right time each month, without major deviations, is one of the signs of good fertility. Having a regular menstrual cycle also means regular ovulation and healthy hormone levels, which makes your fertile window easier to predict.
- Your cervical mucus thickens. The amount and consistency of your vaginal discharge changes throughout your cycle due to hormonal fluctuations. Track these changes while trying to get pregnant—a heavy, wet, slippery discharge resembling raw egg white is a good sign.This usually happens mid-cycle, around the time of ovulation, when your fertility is at its peak.
- Your basal body temperature slightly increases. To check your basal (resting) body temperature, you should measure it each morning as soon as you wake up. Around the time of ovulation, your basal body temperature is likely to increase by 0.5 degrees Fahrenheit. It is a good idea to get a basal body thermometer, which is more sensitive than a regular thermometer.
- You feel pain in your lower stomach. How do I know if I’m ovulating? Ovulation pain, also known as Mittelschmerz, is one of the telltale signs of fertility in women. This benign periovulatory pain happens midcycle for over 40% of ladies of reproductive age. You might feel it in your lower stomach, close to the ovary on the same side as the developing follicle. It happens due to hormonal changes (rise in the levels of LH which triggers ovulation) or as the follicle ruptures and the egg gets released.
- Breast tenderness: Occurs due to hormonal fluctuations, especially an increase in estrogen during ovulation. Breasts feel sore or swollen, indicating that ovulation is approaching.
- Libido changes: Increased libido is common around ovulation, as the body is naturally preparing for conception. A noticeable rise in sexual desire typically occurs mid-cycle, when fertility is at its peak.
@femia.fertility 3 markers of your fertility: cervical mucus, ovulation symptoms, LH test results. Use all the fertility tracking methods in the Femia app and find out the best days to try to get pregnant. #ovulation #fertility #fertilityjourney #lhtest #opk #eggwhitemucus #fertilityapp #fertilitytracker #ovulationsymptoms #ovulationsigns ♬ original sound - Femia fertility app
Tracking fertility: When are you ovulating?
You might be wondering: how do you know how fertile you are? Luckily, you won’t have to rely on just the physical signs of good fertility. Medical tests and evaluations can determine your fertility level.
Ovulation predictor kits
Ovulation predictor kits can detect a surge of LH levels in your urine, which happens around the time of ovulation, and show when your fertility is at its highest. Many women use these kits at home to detect ovulation and make the most of their fertility window.
Ovulation predictor kits can be bought at most drug stores and come with five to seven sticks. You will have to pee on a stick for a few consecutive days—usually three to five—before the expected ovulation date. For instance, if your normal menstrual cycle lasts 28 days, you should start testing on the 11th day after your last period has started.
If your cycle is irregular, talk to your trusted healthcare provider about the timing of the test. The test stick will turn a certain color and display a positive sign if an LH surge is detected.
When to start testing for ovulation
| Cycle length | Day of cycle to begin testing |
|---|---|
| 21 days | Day 5 |
| 22 days | Day 6 |
| 23 days | Day 7 |
| 24 days | Day 8 |
| 25 days | Day 9 |
| 26 days | Day 10 |
| 27 days | Day 11 |
| 28 days | Day 12 |
| 29 days | Day 13 |
| 30 days | Day 14 |
| 31 days | Day 15 |
| 32 days | Day 16 |
| 33 days | Day 17 |
| 34 days | Day 18 |
| 35 days | Day 19 |
| 36 days | Day 20 |
| 37 days | Day 21 |
| 38 days | Day 22 |
| 39 days | Day 23 |
| 40 days | Day 24 |
Hormonal blood testing
To get a better picture of your reproductive health, you can do a blood test that measures the levels of hormones impacting your fertility. Hormonal blood testing must be performed at the right time, due to the changes in hormone levels that come with different phases of the menstrual cycle.
The baseline hormonal blood testing is typically performed at the beginning of the menstrual cycle, usually on the third day of your period. It measures the levels of FSH, LH, and estradiol (a type of estrogen) before they start to increase.
The best time to measure your progesterone levels is in the second half of your cycle (known as the luteal phase), on the 21st day. A rise in progesterone shows that you have ovulated. At this time, you can also recheck the levels of your estradiol, which should have already peaked.
Ultrasound monitoring of follicle development
Ultrasound monitoring of follicles is usually performed together with fertility treatments like ovulation induction or in-vitro fertilization (IVF). It provides insight into the growth and development of follicles (egg-containing sacs) in your ovaries, the health of your reproductive organs, and the timing of ovulation.
Monitoring follicle development is usually performed by vaginal ultrasound starting from the third day of the cycle. Your provider will assess the baseline size, number, and shape of your follicles and check for the presence of any ovarian cysts. As the follicles grow and reach 16 millimeters in size, you might get daily ultrasounds to monitor changes in appearance and the process of ovulation.
Ovarian reserve testing
As a woman, you are born with all the eggs you will have during your lifetime. This is known as the ovarian reserve. As you age and ovulate monthly, the number of follicles decreases—and so does your fertility. Testing the ovarian reserve provides insight into the number of eggs you have left (in comparison with the average for women your age), which helps predict the success of fertility treatments like IVF.
Ovarian reserve testing uses a blood test that measures your FSH levels, as well as the levels of anti-mullerian hormone (AMH) produced by the follicles in your ovaries. FSH is a hormone that makes your follicles grow, and it is typically measured on the third day of your menstrual cycle. Unlike FSH, AMH can be measured at any stage of your cycle. Higher AMH levels suggest a higher number of eggs, and vice versa.
Along with the blood test, your provider might suggest a vaginal ultrasound to estimate your follicle count. They will count the number of visible follicles, typically in the first four days of your menstrual cycle.
👉Find out more: How to improve egg quality: Tips for boosting fertility at any age
Lifestyle factors affecting fertility
Your fertility is not only determined by genetics and medical conditions but also by your lifestyle choices. This is good news! You can monitor the signs your body wants to get pregnant and try to improve your fertility through lifestyle modifications.
A fertility-friendly lifestyle can include changes in your diet, weight, fertility exercise regime, and sleep patterns. Stay away from bad habits such as smoking and drinking.
- Diet and nutrition. A nutrient-rich diet supports healthy hormonal balance and egg quality. The lack of vitamins and minerals such as folic acid, zinc, and antioxidants can meddle with ovulation, and so can basing your diet on processed foods, refined carbohydrates, and trans fats.
- Exercise. Moderate exercise will help you balance your hormones, regulate weight, and reduce stress. Start with moderate cardio activities such as walking, swimming, or cycling, and incorporate strength training to build muscle. Don’t overdo it, though—intense physical activity can also disrupt your menstrual cycle.
- Weight management. Being underweight or overweight can affect hormone production and cause irregular menstrual cycles. Obesity can also lead to conditions such as polycystic ovary syndrome (PCOS) and insulin resistance, which can make it harder to get pregnant. Aim for a body mass index (BMI) between 18.5 and 24.9 for optimal fertility. Losing even 5–10% of body weight can improve your chances of conceiving.
- Sleep quality. Lack of sleep affects the production of hormones like FSH and LH, which may cause your cycle to become irregular. Try to make your sleep schedule as consistent as possible, aim for 7–8 hours of sleep each night, and create a relaxing bedtime routine.
- Stress. Chronic stress is linked to high levels of cortisol, the stress hormone, which can meddle with the release of reproductive hormones and delay or prevent ovulation. Try out relaxation techniques such as deep breathing, meditation, yoga, and mindfulness. Do more of the things you enjoy, such as hobbies and spending time with your loved ones.
- Unhealthy habits. Smoking can damage reproductive organs and reduce your ovarian reserve, while excessive drinking may lead to hormonal imbalances and cycle irregularity. Try to avoid smoking and drinking altogether while trying to conceive. Moreover, drinking too much coffee or other caffeine-packed drinks may also affect your reproductive health, so it is best to limit your caffeine intake to one cup of coffee per day.
👉Find out more: How to boost fertility: 7 natural ways to increase your chances of getting pregnant
Medical condition affecting fertility
Here’s a list of medical conditions that can affect fertility:
Polycystic ovary syndrome (PCOS): A hormonal disorder that can cause irregular ovulation, making it harder to conceive.
Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, causing inflammation, scarring, and infertility.
Tubal blockage: Blocked fallopian tubes can prevent the egg from meeting the sperm, leading to infertility.
Thyroid disorders: Both hypothyroidism and hyperthyroidism can disrupt hormone production and interfere with ovulation.
Uterine fibroids: Non-cancerous growths in the uterus can lead to complications such as miscarriage, preterm birth, or difficulty getting pregnant.
Low sperm count or quality: In men, low sperm count or poor sperm motility can hinder conception.
Pelvic inflammatory disease (PID): An infection of the reproductive organs that can lead to scarring of the fallopian tubes, increasing the risk of infertility.
Premature ovarian failure: Occurs when the ovaries stop functioning normally before the age of 40, leading to anovulation and infertility.
Autoimmune disorders: Conditions like lupus or rheumatoid arthritis can interfere with reproductive health and cause fertility issues.
Diabetes: Poorly controlled diabetes can lead to hormonal imbalances, which may affect ovulation and fertility.
When to seek professional advice
You might have come here wondering, how do I know if I am fertile enough to get pregnant? Maybe you even live a healthy lifestyle and keep a close eye on the signs of your body, but still can’t seem to get pregnant. Sometimes, your journey to motherhood might include a consultation with a trusted healthcare provider or a fertility specialist.
Here is when to seek help:
- If you are under 35 and have been trying for a baby for over a year without success.
- If you are 35 or older and have been trying for six months without success.
- If you are older than 40 and want to get pregnant.
- If your menstrual cycle is irregular (outside of the 21–35 day range).
- If your period is very painful or absent.
- If you have had two or more consecutive pregnancy losses.
- If you have known issues with fertility.
- If your partner has known issues with fertility.
Questions from the Femia community
Can stress affect my fertility?
Yes; research shows that being under a lot of stress can disrupt your menstrual cycle. High levels of stress hormones can meddle with your hormonal balance and disrupt ovulation. Even if it feels like every aspect of your life is giving you a headache, try to find a stress management technique that works for you, such as meditation or exercise.
How does my age impact my fertility level?
As you age (and especially as you pass 35) the number and quality of eggs in your ovaries decreases, as well as your overall fertility. It is an inevitable physiologic process that happens to all ladies approaching menopause. But, don’t be discouraged! It is still possible to get pregnant—it just might take longer. Reach out to your trusted healthcare provider to get personalized advice and come up with a plan.
Can irregular periods mean I’m not fertile?
If your periods vary from month to month, you might be dealing with hormonal imbalances or other health issues that affect fertility. However, women with irregular cycles can still become mothers. It is best to reach out to your trusted healthcare provider to get to the bottom of your unique health situation.
There are a bunch of fertility apps and trackers, can they really help me?
Yes, fertility apps and trackers can help monitor your cycle, predict ovulation, and identify patterns that may improve the chances of conception. However, they are the most accurate when used together with other fertility awareness methods. Pay close attention to the signs of fertility we mentioned.
How many days after your period are you fertile?
You are most fertile 12-16 days before your next period begins, during your ovulation window.
Can you get pregnant outside of your fertile window?
It’s unlikely but possible, as sperm can survive up to 5 days in the reproductive tract, so if you have intercourse before ovulation, you could still conceive.
How long after fertility signs should I try to conceive?
You should try to conceive during the 24-hour period after ovulation signs, as the egg remains viable for about 12-24 hours after release.
The bottom line
While on the journey to pregnancy, there is much to learn about your body. Understanding the hormonal changes that drive your menstrual cycle and looking out for the signs of good fertility can be a game changer.
Listen to your body—track the changes in your basal body temperature, the appearance of vaginal discharge, and even the periovulatory pain you might otherwise ignore. Understanding these cues can help you detect ovulation and periods of high fertility. If you are eager to get pregnant, planning ahead can bring you one step closer to motherhood. Don’t stress and worry; instead, try to live a healthier life and support your reproductive health by making better choices.
If something seems off, know that there is no shame in looking for help. Sometimes, natural conception just needs a little push, while at other times, you might need the assistance of a fertility specialist. Arm yourself with insight, knowledge, and patience. Know that each couple has their own path to parenthood, and even though yours might be a bit different, what matters is the end goal of having your baby in your arms.
References
- Age-Related Fertility Decline – StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK576440/. Accessed 12 Sept. 2024.
- Brott, Nathan R., and Jacqueline K. Le. “Mittelschmerz.” StatPearls, StatPearls Publishing, 2024. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK549822/.
- “Calculating Your Monthly Fertility Window.” John Hopkins Medicine, 20 June 2024, https://www.hopkinsmedicine.org/health/wellness-and-prevention/calculating-your-monthly-fertility-window.
- “Evaluating Infertility.” American Pregnancy Association (ACOG), https://www.acog.org/womens-health/faqs/evaluating-infertility. Accessed 12 Sept. 2024.
- “Fertility Cycle Monitoring: Day 3 and Day 21 Tests.” One Fertility Kitchener Waterloo, 11 May 2022, https://www.onefertilitykitchenerwaterloo.com/fertility-cycle-monitoring-day-3-day-21-tests/.
- “Fertility Explained.” VARTA, https://www.varta.org.au/understanding-fertility/fertility-explained. Accessed 12 Sept. 2024.
- Holesh, Julie E., et al. “Physiology, Ovulation.” StatPearls, StatPearls Publishing, 2024. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK441996/.
- Jha, Praveen. “Follicular Monitoring | Radiology Reference Article | Radiopaedia.Org.” Radiopaedia, https://doi.org/10.53347/rID-26295. Accessed 12 Sept. 2024.
- Kala, Manika, and Manish Nivsarkar. “Role of Cortisol and Superoxide Dismutase in Psychological Stress Induced Anovulation.” General and Comparative Endocrinology, vol. 225, Jan. 2016, pp. 117–24. ScienceDirect, https://doi.org/10.1016/j.ygcen.2015.09.010.
- “Ovarian Reserve Testing: Range, Purpose & Results.” Cleveland Clinic, https://my.clevelandclinic.org/health/diagnostics/25142-ovarian-reserve-testing. Accessed 12 Sept. 2024.
- “Ovulation Home Test.” MedlinePlus, https://medlineplus.gov/ency/article/007062.htm. Accessed 12 Sept. 2024.
- Physiology, Menstrual Cycle – StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK500020/. Accessed 12 Sept. 2024.

The 5-5-5 rule is a simple guideline for the first 15 days postpartum which can help with recovery following childbirth. It encourages intentional rest while bonding with your baby.
Discover what happens at 35 weeks pregnant, from baby development and symptoms to concerns about sex and breastfeeding benefits.

Discover safe and comfortable sex positions during pregnancy that enhance intimacy while accommodating bodily changes. Explore positions that prioritize comfort and intimacy, ensuring both partners feel connected and at ease.

