Femia > Health Library > Getting Pregnant > Trying to conceive > Can you get pregnant during perimenopause?
Can you get pregnant during perimenopause?

- Updated Feb 11, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
Ovulation during perimenopause becomes sporadic due to fluctuating hormone levels, significantly decreasing its frequency. While pregnancy is still possible until menopause is confirmed, ovulation often requires medical monitoring for accurate detection.
Pregnancy during perimenopause carries higher risks, including complications like preeclampsia, gestational diabetes, thrombosis, chromosomal abnormalities, and premature birth. Maternal age also increases the risk of labor complications. If trying to conceive or avoid pregnancy, consult a healthcare provider for guidance.
If I’m still having periods at 55, can I get pregnant? We have comforting news for those of you looking to get pregnant later in life: pregnancy is still possible during this transitional period.
While many people assume fertility ends with the start of perimenopause, the reality is much more complex. Although your hormones tend to fluctuate and cause irregular menstrual cycles, sporadic ovulation can still occur. This means conception is not entirely off the table.
Let’s explore the way your fertility changes during perimenopause, how to detect ovulation and increase your chances of getting pregnant, as well as what this potential pregnancy might look like.
Femia offers the most accurate tool for determining ovulation and fertile days
How perimenopause affects fertility
Perimenopause is a time of hormonal shifts in the female body. What does that mean for your fertility and chances of conception?
Fluctuating levels of estrogen and progesterone will likely cause irregularities in your ovulation and menstrual cycle. You might ovulate as usual some months, while in others you may not ovulate at all. Your periods might come closer together, farther apart, or even skip entirely.
At this stage of life, the number and quality of your eggs will likely have decreased. This means your fertility is naturally declining, on top of hormonal changes. Still, some women experience both perimenopause and pregnancy at 50.
@femia.fertility Dreaming of a faster way to get pregnant? 🤰✨ Femia's got you covered with the smoothest path to natural pregnancy! Be part of our growing community of 500k+ women worldwide who've achieved their dreams with us. Download Femia app and let's start your journey!💕 #tryingtoconceive #ttcjourney #fertilityjourney #pregnancyover30 ♬ original sound - Femia fertility tracker
Can you get pregnant during menopause?
To provide the right answer to this question, we will first have to unpack the difference between menopause and perimenopause. Although these two stages of female reproductive health may feel similar, they are very different.
Perimenopause is a period before full menopause, marked by hormonal changes, infrequent ovulation and periods, and a decline in fertility. It might last for a few months to a decade, although it’s most often three to four years long. Menopause is a time in your life marked by no periods for 12 months. During perimenopause, women may also experience specific symptoms such as hot flashes, night sweats, and emotional changes, which can impact overall well-being.
So, can you get pregnant during menopause? It’s really simple: menopause is defined as 12 consecutive months without periods, after which pregnancy is no longer possible. However, during the early transitional phase before menopause is fully established (perimenopause), ovulation might still occur. This means that even if you haven’t had a period in a while, there is still a chance of pregnancy, so it’s important to be cautious if you’re not trying to conceive.
👉 Find out more: My husband takes testosterone injections. Can I still get pregnant
Signs of ovulation during perimenopause
As you go into perimenopause, it might become more difficult to tell when you are ovulating. Symptoms of ovulation might occur unexpectedly or not at all. Here is how to detect ovulation:
- Changes in cervical mucus. Your cervical mucus may appear inconsistent or less abundant compared to earlier years, making it harder to predict ovulation. Despite hormonal fluctuations, you may still notice that it becomes clear, stretchy, and slippery around ovulation, indicating a fertile window.
- Ovulation pain. You could still experience mild pelvic pain (mittelschmerz) at the time of ovulation, even if cycles are irregular.
- Your basal body temperature rising. A slight increase in basal body temperature (about 0.5–1°F) after ovulation may still occur, though tracking might be less reliable due to irregular ovulation.
- Irregular periods. Your periods may become shorter, longer, or skip months entirely. You might also notice mid-cycle spotting or unusually heavy or light periods, because of hormonal shifts happening in your body.
- Pregnancy-like symptoms. Sometimes, hormonal fluctuations can mimic early pregnancy symptoms, such as tender breasts, bloating, or mood changes.
Common myths about perimenopause and pregnancy
There are many misconceptions about pregnancy during perimenopause. Let’s discuss a couple of them.
Myth 1: You can’t get pregnant if your periods are irregular
Even if your menstrual cycle is unpredictable during perimenopause, ovulation can still happen sporadically. While irregular cycles make it harder to track ovulation and predict the fertile window, they don’t eliminate the chance of pregnancy. Although the chances are low, you could still get pregnant.
Fact 1: You can get pregnant until menopause
Pregnancy is possible whenever an egg is released. Irregular cycles significantly complicate predicting the fertile window, so although the chances are low, pregnancy is still possible. If you’re not actively trying to conceive and want to avoid pregnancy, it’s important to use contraception consistently until menopause is confirmed, which is marked by 12 consecutive months without a period.
Myth 2: Age guarantees infertility
While fertility does decline with age, it doesn’t disappear entirely until menopause. The quality and quantity of eggs decrease over time, making conception more difficult, but older women can still be fertile during perimenopause, when hormonal changes allow occasional ovulation.
Although age reduces fertility, modern reproductive technologies, such as egg donation or IVF, can significantly increase the chances of pregnancy for women of advanced age who wish to have children later in life.
Fact 2: Older women may still get pregnant
Women in their 40s and even early 50s can still ovulate and become pregnant, though it may be less likely than in their younger years. Advances in reproductive healthcare, such as fertility treatments, can also help you conceive if desired.
Pregnancy during perimenopause: What you need to know
Pregnancies at a later stage in life come with a unique set of challenges. Here is what you need to know to prepare yourself for the journey.
- Pregnancy symptoms might be more intense. The usual pregnancy symptoms like fatigue, nausea, and mood swings might get more extreme due to fluctuating hormones.
- You will need appropriate medical attention. If you get pregnant during perimenopause, your healthcare provider will want to monitor your pregnancy closely. You will likely attend frequent prenatal checkups and receive specialized care if any complications arise. Regular monitoring of both maternal and fetal health, including Doppler ultrasound and screening tests, is critically important for pregnancies at an advanced maternal age to ensure the well-being of both mother and baby.
- You will need support. You might have to balance pregnancy with other responsibilities, such as work, family, or older children. It’s completely normal to have feelings of worry or anxiety about raising a child later in life. As you go through this journey, it helps to have the support of your partner, family, and friends.
Femia offers the most accurate tool for determining ovulation and fertile days
Risks of getting pregnant during perimenopause
Is it dangerous to get pregnant during perimenopause? Pregnancy during perimenopause is tied to higher health risks for both the mother and the baby. If you are looking to get pregnant later in life, it’s important to understand these risks in order to make an informed decision.
Health risks for mothers
- High blood pressure. Older women are at a higher risk of developing high blood pressure during pregnancy, which can lead to complications like preeclampsia, a condition characterized by high blood pressure and organ damage. Your healthcare provider will monitor your condition closely and may advise you to make lifestyle changes, like eating a healthy diet and stressing less.
- Gestational diabetes. As women age, their risk of developing gestational diabetes, a form of diabetes that develops during pregnancy, increases. This condition can lead to complications such as excessive weight gain, preterm birth, and an increased risk of developing type 2 diabetes later in life for both mother and child. Managing gestational diabetes typically involves dietary changes, regular exercise, and close monitoring of blood sugar levels.
- Increased risk of miscarriage. Women over 40 may face a significantly higher risk of pregnancy loss in the early stages, often due to issues with fetal development. This is due to the decline in egg quality and the higher likelihood of chromosomal abnormalities, such as Down syndrome. Getting genetic counseling and focusing on early prenatal care to assess these risks might be a good idea.
Risks to the baby
- Chromosomal abnormalities. Babies conceived later in life face increased risks of genetic conditions, intrauterine growth restriction (IUGR), and complications due to placental insufficiency, which can affect their development and overall health. These risks can be detected early through prenatal testing, such as noninvasive prenatal testing (NIPT), amniocentesis, or chorionic villus sampling (CVS).
- Premature birth. Perimenopause babies are more likely to be born early (before 37 weeks of pregnancy), which might cause complications like underdeveloped lungs, feeding difficulties, and long-term developmental delays.
- Low birth weight. Babies born to older mothers may be smaller than average due to reduced placental function or other pregnancy complications.
Lifestyle and emotional considerations
Having a baby later in life is always a challenge, even if you‘ve dreamed of becoming a mother for a long time. You might face uncertainty and anxiety about the health risks we just discussed, and that is perfectly fine. It’s okay to feel both joyful and worried about this new chapter in your life.
The journey might require some adjustment in your daily life, as well. Babies are tiring—especially during the first couple of years. Balancing your career and parenting as you age can be challenging, but take your time, and seek support when you need it. With proper support and planning, these challenges can be managed, making the experience a positive and empowering one.
Can I increase my chances of getting pregnant during perimenopause?
If you are looking to get pregnant during perimenopause, here is what you can do to increase your fertility:
- Track your ovulation. This is the key first step, even if cycles are irregular. You can track ovulation by monitoring physical signs, like cervical mucus, using ovulation predictor kits, and writing it all down in the Femia app.
- Maintain a healthy lifestyle. Focus on getting your body to a good place with proper nutrition, regular exercise, stress management, and avoiding harmful habits, like smoking or excessive alcohol consumption.
- Consult a fertility specialist. It’s a good idea to talk to a healthcare provider or fertility specialist early on in the process. They can help identify potential challenges, recommend appropriate tests, and guide you toward personalized strategies for getting pregnant.
Although the chances of getting pregnant decrease with age, there is still hope. If you are struggling with natural conception, medical interventions, like in-vitro fertilization (IVF), can be another option. Other interventions, such as hormone therapy or intrauterine insemination (IUI), may also be considered based on your individual needs.
👉Find out more: When to have sex during ovulation: Your guide to maximizing fertility
Safe birth control options for perimenopause
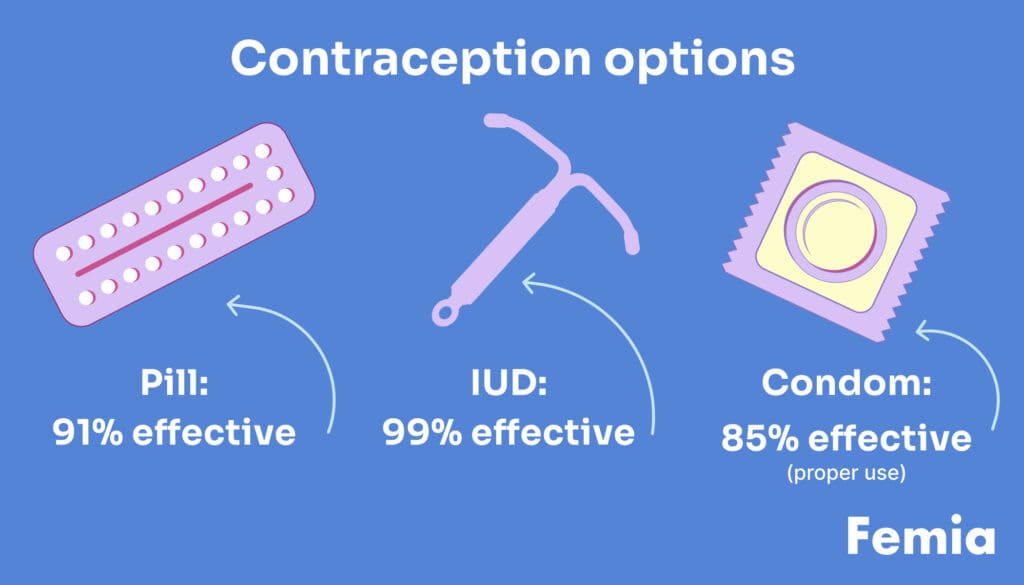
If you are not looking to get pregnant during perimenopause, don’t forget about contraception. Relying on irregular cycles as a form of birth control is highly risky. The chances of unintended pregnancy are higher without using barrier methods or hormonal contraceptives, which are strongly recommended for effective pregnancy prevention. Talk with your trusted healthcare provider to choose the most suitable method, ensure peace of mind, and avoid unnecessary complications.
- Intrauterine devices (IUDs). Long-term, hassle-free protection available in hormonal and non-hormonal forms.
- Hormonal contraceptives. Birth control pills and other hormonal contraceptives not only prevent pregnancy but may also help regulate periods, reduce heavy bleeding, and alleviate symptoms like hot flashes.
- Non-hormonal methods. If hormonal birth control methods don’t appeal to you, consider a copper IUD or rely on single-use methods, like condoms or diaphragms.
Every woman’s needs are unique, so exploring the benefits and drawbacks of each option with a healthcare provider will ensure your choice aligns with your lifestyle and health goals.
When to consult a doctor
It’s always a good idea to consult a doctor for personalized guidance on family planning, fertility management, and birth control options.
A healthcare provider can help assess your reproductive health, explain how to navigate fertility during perimenopause, and recommend the most effective contraceptive methods tailored to your needs. They can also provide support if you’re considering pregnancy, offering advice on lifestyle changes, fertility tracking, and potential medical interventions.
Make sure to seek medical attention if you experience irregular periods that disrupt your life, suspect symptoms of pregnancy, or face difficulty conceiving despite trying for several months.
Questions from the Femia community
Can I get pregnant if I’m on hormone replacement therapy?
Hormone replacement therapy might help you manage perimenopause symptoms like hot flashes and mood swings, but it is not a form of contraception. You can still get pregnant until menopause is confirmed, so make sure to use protection alongside hormone replacement therapy if you want to avoid pregnancy.
Can I still get pregnant if I’m having irregular periods?
Irregular periods during perimenopause can make it harder to predict ovulation, but they do not eliminate the possibility of pregnancy. Even if your cycles are inconsistent or infrequent, ovulation can still occur, and pregnancy is possible if an egg is released and fertilized.
Should I use birth control if I’m 55 and still menstruating?
As long as menstruation continues, even if it’s irregular, there’s still a chance of ovulation and, therefore, pregnancy. If you don’t want to get pregnant, use a reliable form of birth control until menopause is officially confirmed, after 12 consecutive months without a period.
Is it safe to have a baby at 50?
Having a baby at 50 does come with inherent health risks, including an increased chance of complications like high blood pressure, gestational diabetes, chromosomal abnormalities, and premature birth. However, with proper medical supervision, including early prenatal care and close monitoring throughout the pregnancy, you can still have a successful pregnancy.
The bottom line
Pregnancy during perimenopause is possible but comes with unique challenges and risks for both mother and baby. If you are looking to get pregnant at a later stage in life, it is best to reach out to your trusted healthcare provider for personalized guidance.
For those of you not interested in getting pregnant, it is important to understand your fertility during this transitional time. As long as you still get your period, pregnancy is possible. Don’t skip out on birth control or other forms of contraception just because of irregular periods.
References
- Brott, Nathan R., and Jacqueline K. Le. “Mittelschmerz.” StatPearls [Internet], StatPearls Publishing, 2023. www.ncbi.nlm.nih.gov, https://www.ncbi.nlm.nih.gov/sites/books/NBK549822/.
- Glick, Itamar, et al. “Management of Pregnancy in Women of Advanced Maternal Age: Improving Outcomes for Mother and Baby.” International Journal of Women’s Health, vol. 13, Aug. 2021, pp. 751–59. PubMed Central, https://doi.org/10.2147/IJWH.S283216.
- Grandi, Giovanni, et al. “Contraception During Perimenopause: Practical Guidance.” International Journal of Women’s Health, vol. 14, July 2022, pp. 913–29. PubMed Central, https://doi.org/10.2147/IJWH.S288070.
- “Menopause.” The National Health Service (NHS), 23 Oct. 2017, https://www.nhs.uk/conditions/menopause/.
- Perimenopause. 2 Dec. 2024, https://www.hopkinsmedicine.org/health/conditions-and-diseases/perimenopause.
- “Perimenopause: Rocky Road to Menopause.” Harvard Health, 9 June 2009, https://www.health.harvard.edu/womens-health/perimenopause-rocky-road-to-menopause.
- “Periods and Fertility in the Menstrual Cycle.” Nhs.Uk, 9 Apr. 2018, https://www.nhs.uk/conditions/periods/fertility-in-the-menstrual-cycle/.
- “Trying to Get Pregnant? Here’s When to Have Sex. | ACOG.” The American Colleage of Obstetricians and Gynecologists (ACOG), https://www.acog.org/womens-health/experts-and-stories/the-latest/trying-to-get-pregnant-heres-when-to-have-sex. Accessed 19 Dec. 2024.

Not sure you’re experiencing Plan B spotting vs implantation bleeding? Learn how to tell the difference based on timing, flow, and symptoms.

At 28 weeks pregnant, you’re entering the third trimester. Learn about baby size, symptoms, ultrasound, and health tips for a smooth journey.

Discover the complete parent’s guide to shaken baby syndrome’s causes, symptoms, prevention, and misconceptions.

