Femia > Health Library > Pregnancy > Giving birth > C-section vs vaginal birth: What to know about benefits, risks, and recovery
C-section vs vaginal birth: What to know about benefits, risks, and recovery
- Updated Feb 10, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
C-sections and vaginal births offer different risks and benefits. C-sections have a longer recovery time; for some women, however, it is the safest way to give delivery.
When deciding on whether to have a C-section or vaginal birth, your medical history, pregnancy, and personal preference can all influence your decision. Talk to a trusted healthcare provider about the risks and benefits of each option for you and your baby to guide your decision.
At around 37–40 weeks of pregnancy, your baby is ready to exit your womb and enter the world. You can give birth in one of two ways: vaginally or through a surgical procedure called a cesarean section (C-section). The main goal for both is to ensure the safety and health of you and your baby.
As you begin thinking about how you’d like to give birth, understanding the differences between vaginal births and C-sections, including the risks and benefits of each, can help you to decide. Listening to medical advice and factoring in your unique circumstances will allow you to choose the best path for you and your baby.
Join thousands of moms-to-be who trust Femia for expert-backed
guidance during pregnancy and beyond
What is the difference between C-sections and vaginal births?
A vaginal birth is the natural process of delivering your baby through the vagina. While all vaginal births involve the process of the baby passing through the birth canal, the amount of medical support you can have will vary, depending on preference and personal circumstances.
Here are some key ways vaginal births can differ:
- Where you give birth. You can have a vaginal birth at home, in a birthing center, or at a hospital. However, home births are recommended only for low-risk pregnancies and should be attended by a certified midwife or doula, under international standards such as those from NICE or ACOG. These guidelines ensure that the birth process is closely monitored and that necessary medical support is available if complications arise.
- How you give birth. Depending on circumstances and preference, there are different positions you can give birth in. For example, you can give birth in a birthing pool, on all fours, or lying in a bed.
- What pain relief you have. There are several options to help manage labor pain, including a TENS machine, gas and air, opioids, and epidurals. Some women will prefer not to have any pain relief.
- Other medications. You might be offered medication to get labor started (induction) or to speed it up if things are stalling. This is based on personal circumstances and medical advice.
- If you need help getting the baby out of the birth canal. Some women will have an ”assisted birth”—this is where a suction cap (vacuum) or forceps are used to help pull the baby out of the vaginal canal.
- Episiotomy. An episiotomy is a surgical cut made in the perineum (the area between the vagina and anus) to widen the vaginal opening. This is sometimes done if an assisted birth is required, to prevent a severe tear, or when the baby needs to be born quickly. However, routine episiotomy is not recommended according to modern standards and guidelines, except in cases where it is medically justified, such as when there is a direct threat of fetal hypoxia or stillbirth.
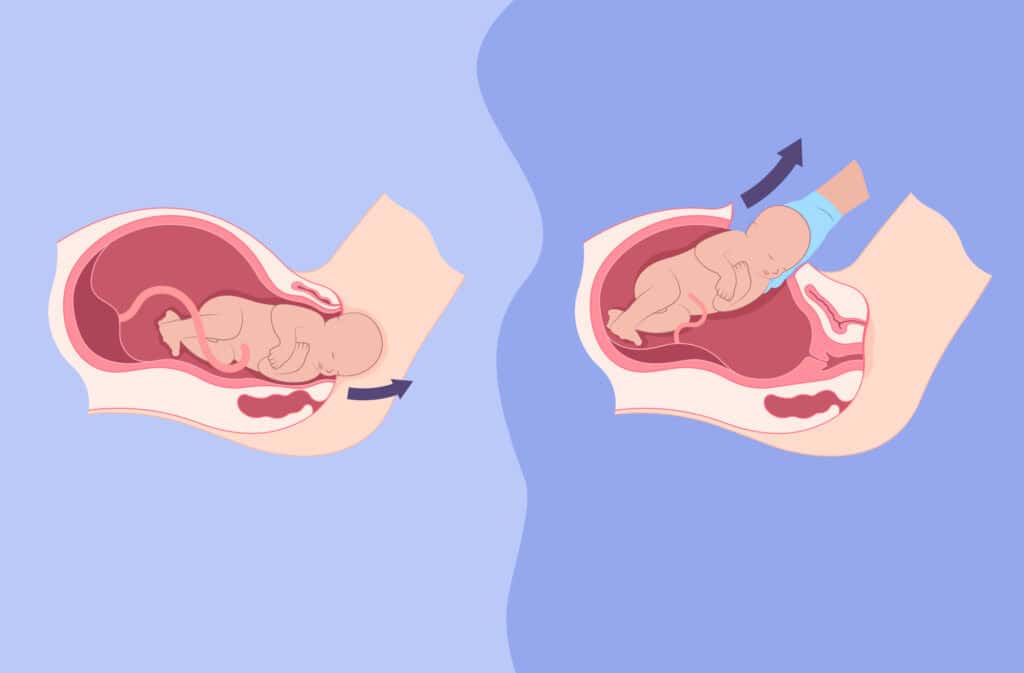
A C-section is a surgical procedure that is performed to deliver the baby through the abdomen (tummy). A surgeon who specializes in caring for pregnant women and delivering babies (obstetrician) will perform the C-section in a hospital.
👉Find out more: When should you go to the hospital for labor? Key signs to watch out for
Two types of C-sections you can have
- Planned (elective) C-section. A planned C-section is scheduled in advance, with the operation usually taking place after 39 weeks of pregnancy unless medical reasons require an earlier procedure. ACOG and RCOG recommend waiting until 39 weeks to reduce risks like respiratory distress in the baby. Early C-sections may be necessary in cases such as placenta previa, severe preeclampsia, or risk of uterine rupture.
- Emergency C-section. This is when a vaginal birth was planned but for medical reasons, it’s been decided that a C-section is the safer option. This can happen either before labor has started, at the beginning of labor, or after you have been in labor for a while. Emergency C-section may be necessary in cases of fetal distress, such as abnormal heart rhythms, acute hypoxia or asphyxia, severe preeclampsia or eclampsia, umbilical cord prolapse, or when labor progress is stalled with ineffective cervical dilation or fetal descent.
| What to expect during a C-section:
• Most women remain awake, with a spinal or epidural anesthetic ensuring that you’re completely numb from the waist down. • Occasionally, a general anesthetic might be used to put you to sleep during the procedure. • A 10–20cm cut will be made across your lower tummy and uterus. • The procedure usually takes under an hour. • If your baby is well, then you will be able to see and hold them as soon as they’ve been delivered. |
Reasons for having a C-section
There are many reasons why a woman might have a C-section, including both medical reasons and personal preference. In some cases, a C-section is the safest way to give birth and can be lifesaving for both the mother and baby. Here are some reasons why you might have a C-section:
- Your baby is not in a head-down position. If your baby is lying breech (bottom down) or transverse, then a C–section is usually the safest way to deliver.
- You’re carrying more than one baby. Carrying two or more babies might mean your healthcare provider recommends a C-section.
- There is a problem with the placenta. Sometimes, the placenta can cover the opening of the cervix (placenta previa), making it dangerous to attempt a natural birth.
- Prolapsed umbilical cord. If some of the umbilical cord has prolapsed through the cervix, then a C-section might be recommended.
- Health problems with the mother. If you have a medical condition that puts your health at risk by going through natural labor, then your healthcare professional will likely recommend a C-section.
- Previous C-section. It’s possible to have a vaginal birth after a C-section (VBAC) but, depending on the reason for your C-section, it might not be advised.
- Problems during labor. If the baby becomes distressed, labor is moving too slowly, or other problems arise during a natural vaginal birth, your healthcare provider might recommend an emergency C-section. At times, this can be lifesaving.
How long does it take to recover from a C-section vs a vaginal birth
Recovery will differ from woman to woman and will greatly depend on individual circumstances, like underlying health and if there were any complications during childbirth. However, in general, it takes longer to recover from a C-section than from a vaginal birth.
According to the American College of Obstetricians and Gynecologists (ACOG), most women who have a C-section will stay in hospital for 2–4 days after giving birth, whereas for a vaginal birth, it’s around 24 hours. If you’ve had a C-section, you might also be advised to limit activities like heavy lifting and driving for the first 6-8 weeks while your surgical incision heals.
C-section vs vaginal birth: Which is more painful?
Pain levels will vary for everyone, as pain is subjective; however, here’s what you can typically expect:
- Vaginal birth: More intense pain during labor and delivery but a shorter and less painful recovery. If you had a vaginal tear or episiotomy, then you could have some vaginal pain for a few weeks; however, this should be manageable with basic painkillers and simple care methods, like sitting on a padded ring and using cooling packs on the wound.
- C-section: You shouldn’t feel any pain or discomfort during the procedure itself but, like with any abdominal surgery, you will likely experience some pain for a couple of days afterward. You should be offered painkillers to help with this. As your wound heals, you might have to avoid some activities until you have had your six-week postpartum check-up with your healthcare provider.
C-section vs normal delivery pros cons
Both types of childbirth have their own pros and cons. Your decision will ultimately depend on your personal circumstances and medical advice. Here’s a quick look at the advantages and disadvantages of C-sections and vaginal deliveries.
| Type of delivery | Pros | Cons |
|---|---|---|
| C-section | • Control over scheduling (if planned)
• In certain circumstances, it can be lifesaving for a mother and baby • Safer than vaginal birth in certain medical situations • Avoids complications from vaginal birth and long labor (eg. vaginal tears, urinary incontinence, pelvic organ prolapse) • Having a planned C-section avoids needing an emergency C-section | • Average stay in hospital longer than a vaginal delivery
• More pain after delivery than vaginal birth • Longer recovery time than vaginal birth • Higher risk of severe complications to mother and baby, including postpartum infection and maternal death • Potentially impacts future pregnancies (eg. uterine rupture risk) • May disrupt breastfeeding to begin with • Babies born via C-section could be at higher risk of having breathing problems at birth and later in life such as asthma, especially if the birth occurred before 39 weeks (in the case of a planned C-section). • Small chance of a baby being injured by the scalpel during the procedure • Risk of infection from surgical incision • When the wound from the C-section heals, you will have a post-surgery scar in your lower abdomen |
| Vaginal delivery | • The average stay in hospital is shorter
• Shorter recovery time and less pain after labor • Avoids surgical risks from major abdominal surgery • No abdominal scar • Baby less likely to suffer breathing problems after birth | • Can be very long and physically grueling
• Can be very painful during labor and delivery • Risk of vaginal/perineal tearing • Risk of needing an episiotomy • Higher risk of urinary incontinence and pelvic organ prolapse • Risk of needing and emergency C-section and, therefore, all of the associated surgical risks • Risk of baby being injured during birth (eg. shoulder injuries) |
Why is natural birth better than a C-section for the baby?
A natural birth can be better than a C-section if you have a complication-free pregnancy, your baby is head down, and there are no other risks. While it’s impossible to predict the future, in an uncomplicated delivery, a natural vaginal birth can offer your little one some unique advantages:
- Natural compression of the baby as it passes through the vaginal canal helps to expel amniotic fluid from its lungs. This doesn’t happen during a C-section and, for some babies, especially those born before 39 weeks, it can result in temporary breathing difficulties. These can be managed in the hospital and usually improve after a few days.
- The hygiene hypothesis. Exposure to vaginal bacteria during a vaginal birth might be beneficial to the baby in the long run. A 2019 systematic review and meta-analysis examined 39 studies exploring the link between C-sections and childhood asthma. It found that children delivered via C-section were more likely to develop childhood asthma compared to those born vaginally. The study theorized that this could be due to the baby not being exposed to beneficial microbes in the vaginal canal. However, this remains a hypothesis, and most experts agree more research is needed to confirm or deny the link.
- Lower risk of maternal complications. A recent 2024 study published in the American Journal of Perinatology looked at over 400,000 deliveries and found that women who had a C-section were twice as likely to have experienced a severe complication in the first 42 days after giving birth. However, the study didn’t differentiate between emergency and planned C-section, which may have impacted the results.
Is a C-section safer than a natural birth?
Whether a C-section or a natural birth is safer for you and your baby will depend on your unique circumstances. For an uncomplicated pregnancy, where the baby is in a head down position and the mother has no health concerns, then having a vaginal birth is generally considered the safer option. However, a C-section is a common surgical procedure that generally has a good safety record. In some circumstances, it can be the safest option for mother and baby.
Stomach after C-section vs natural birth: Recovery and appearance
The appearance and recovery of your stomach after C-section or natural birth can vary:
- C-section: You will have a scar on your lower abdomen. To begin with, it can be quite obvious, but it should fade with time. Healing can also take longer, as a C-section is abdominal surgery, and the muscles and layers of your abdomen will need some time to heal.
- Vaginal birth: the recovery should be quicker, but you may experience problems with your pelvic floor, including urinary incontinence and pelvic organ prolapse. This can occur both soon after childbirth and many years down the line.
To help your body recover after childbirth, here are a few ways to care for your body after you’ve given birth:
- If you have a vaginal birth, using cooling pads around your perineum can ease any pain you might have, especially if you had a tear. Practicing pelvic floor exercises like Kegels or visiting a physiotherapist who specializes in women’s pelvic floor muscles can help you strengthen your pelvic floor and prevent any long-term issues. However, it is recommended to start pelvic floor exercises only after receiving approval from your doctor, especially if there were significant tears or an episiotomy in the postpartum period.
- For C-section recovery, make sure you avoid heavy lifting, use the recommended pain relief, keep the incision area clean and dry, and avoid sex and exercise for at least 6 weeks, or until your healthcare provider has given you the all-clear, depending on the condition of your incision.
In both cases, it is important to follow postpartum recommendations and prioritize rest, hydration, and good nutrition where possible.
👉Find out more: Postpartum essentials for mom: A complete checklist for recovery
Benefits of planned C-section
For some women, a planned C-section is the best choice for them and their baby. Your healthcare provider might recommend a C-section due to medical reasons, or you might decide that this is the right decision for you for other reasons. Here are some of the benefits of a planned C-section:
- Avoiding labor pain and unpredictability. Many women opt for a planned C-section due to concerns about the pain and unpredictability of labor. If you have explored your concerns with your healthcare provider, been informed of the risks and benefits, and feel that this is the right choice for you, then a planned C-section can help you feel more relaxed and in control of your birth.
- Control over the date. While it’s unlikely that your healthcare provider will advise you to have a non-medically necessary C-section earlier than 39 weeks, it still enables you to choose the day. This can help parents plan around specific events, like important family or work commitments.
- Medically necessary. If a vaginal birth poses risks, your healthcare provider may recommend a planned C-section. This decision will be made only when the benefits outweigh the risks. While it can be disappointing if you were hoping for a vaginal birth, it might be the safest option for both you and your baby.
While planned C-sections have benefits, it’s important that you weigh them against the risks and recovery considerations. Your healthcare provider will be able to help guide you.
Choosing the right delivery method for you
Choosing whether to have a C-section or a vaginal birth is a highly personal decision and will depend on several factors, including your medical history, any pregnancy conditions, and personal preference.
If you are considering a planned C-section or have concerns about having a vaginal birth, reach out to your healthcare provider. They will be able to take a personalized approach, discuss the pros and cons of each option with you, and help you to make an informed decision that is right for you and your baby.
Join thousands of moms-to-be who trust Femia for expert-backed
guidance during pregnancy and beyond
Questions from the Femia сommunity
Can I have a vaginal birth after a C-section?
Yes, VBAC (vaginal birth after cesarean) is possible, and safe, for many women. But, it depends on factors like uterine health and the reason for the previous C-section. If you are pregnant again after having a C-section and would like to explore the possibility of a vaginal birth, your healthcare provider will be able to offer you personalized guidance about the risks and benefits of a VBAC.
Are there risks of having multiple C-sections?
Yes, risks increase with each C-section, including scar tissue buildup, placenta accreta, and uterine rupture. Each additional C-section can become more challenging, and the recovery can be longer and more painful.
Does a C-section affect breastfeeding?
A C-section won't prevent you from breastfeeding, but it can make it more challenging to start with. Factors like recovery pain, delayed milk production, or delayed skin-to-skin contact can all play a role. However, with some support and guidance, many women successfully breastfeed after a C-section.
Is a planned C-section covered by insurance?
Coverage depends on the healthcare provider and country; planned C-sections without medical necessity may not always be covered. Always check with your healthcare provider and insurance company about the conditions surrounding a planned C-section, if you’re considering one, to avoid any nasty surprises down the line.
The bottom line
However you give birth, the main aim will always be to ensure yours and your baby’s health. While risks and benefits, recovery time, and time it takes to give birth can vary widely between C-section and vaginal delivery, with proper medical care, both methods overwhelmingly result in a healthy delivery.
For some women, a C-section will be the right decision, whether due to a medical condition that makes a vaginal birth unsafe or other personal reasons. Whatever your situation, discussing the pros and cons with your healthcare provider first can help you make an informed decision and prepare for childbirth in the best way possible.
References
- After Vaginal Delivery – in the Hospital: MedlinePlus Medical Encyclopedia. medlineplus.gov/ency/patientinstructions/000629.htm.
- Author, Femia. “Postpartum Essentials for Mom: Thighs to Prepare in Advance | Femia.” Femia Health, 2 Oct. 2024, femia.health/health-library/being-a-mom/recovering/postpartum-essentials-for-mom.
- “Cesarean Birth.” ACOG,
- www.acog.org/womens-health/faqs/cesarean-birth#maincontent.
- C-section – Mayo Clinic. www.mayoclinic.org/tests-procedures/c-section/about/pac-20393655.
- Darabi, Behzad, et al. “The Association Between Caesarean Section and Childhood Asthma: An Updated Systematic Review and Meta-analysis.” Allergy Asthma and Clinical Immunology, vol. 15, no. 1, Oct. 2019, https://doi.org/10.1186/s13223-019-0367-9.
- Doherty, Brett, et al. “Maternal and Infant Morbidity and Mortality in Relation to Delivery Mode in a Large US Healthcare Claims Database in 2019 and 2020.” American Journal of Perinatology, Sept. 2024, https://doi.org/10.1055/a-2419-8916.
- “How to Squeeze in Kegels All Day Long.” Mayo Clinic, www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/kegel-exercises/art-20045283.
- Keag, Oonagh E., et al. “Long-term Risks and Benefits Associated With Cesarean Delivery for Mother, Baby, and Subsequent Pregnancies: Systematic Review and Meta-analysis.” PLoS Medicine, vol. 15, no. 1, Jan. 2018, p. e1002494. https://doi.org/10.1371/journal.pmed.1002494.
- Mascarello, Keila Cristina, et al. “Maternal Complications and Cesarean Section Without Indication: Systematic Review and Meta-analysis.” Revista De Saúde Pública, vol. 51, Nov. 2017, p. 105. https://doi.org/10.11606/s1518-8787.2017051000389.
- “Placenta Previa – Symptoms and Causes – Mayo Clinic.” Mayo Clinic, 11 May 2022, www.mayoclinic.org/diseases-conditions/placenta-previa/symptoms-causes/syc-20352768.
- Prior, Emily, et al. “Breastfeeding After Cesarean Delivery: A Systematic Review and Meta-analysis of World Literature.” American Journal of Clinical Nutrition, vol. 95, no. 5, Mar. 2012, pp. 1113–35. https://doi.org/10.3945/ajcn.111.030254.
- Website, Nhs. “Episiotomy and Perineal Tears.” nhs.uk, 14 Nov. 2024, www.nhs.uk/pregnancy/labour-and-birth/what-happens/episiotomy-and-perineal-tears.
- “What Are Some Common Complications During Labor and Delivery?” https://www.nichd.nih.gov/, 1 Sept. 2017, www.nichd.nih.gov/health/topics/labor-delivery/topicinfo/complications#main-content.
- “What You Can Expect After a Vaginal Delivery.” Mayo Clinic, www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/postpartum-care/art-20047233.

Discover key signs your body is ready for pregnancy. Learn how to know if you’re fertile enough to get pregnant: physical indicators, medical tests, etc. Expert advice from Femia.
At 9 weeks pregnant, your baby is now moving and growing fast! Find out about symptoms, baby size, and how to care for yourself this week.
Kansas has filed a lawsuit against Pfizer, alleging misinformation about its COVID-19 vaccine’s safety and effectiveness, including during pregnancy. Learn more about the claims, evidence, and implications.

