Femia > Health Library > Pregnancy > Giving birth > Late decelerations during labor: What you need to know
Late decelerations during labor: What you need to know
- Updated Feb 10, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
Late decelerations during labor, a gradual drop in the baby’s heart rate after contractions, indicate potential issues with placental blood flow and require immediate medical attention. Nursing interventions include repositioning the mother, administering oxygen, and potentially delivering the baby via C-section if necessary.
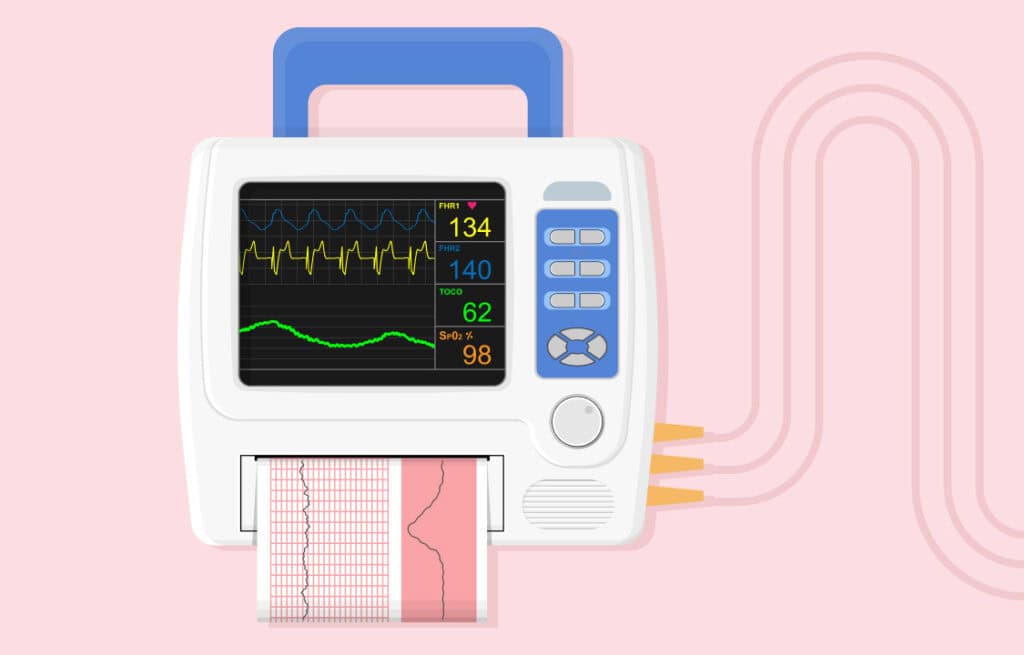
You may already know that doctors monitor a baby’s heart rate during pregnancy. The same happens during labor. The key goal of monitoring a baby’s heart rate is to find any abnormalities, and one of them might be late decelerations. This means a gradual drop in the baby’s heart rate due to a lack of placental blood flow.
While late decelerations are common and doctors know how to manage them in the majority of cases, this abnormality may still have negative long-term consequences, especially if the medical staff does not properly and quickly handle it.
What do late decelerations mean?
As mentioned above, late decelerations refer to a gradual drop in the baby’s heart rate and are important to keep an eye on. Healthcare providers use electronic fetal monitoring to record the heartbeat of the fetus as well as the mother’s contractions before and during labor.
Fetal decelerations are divided into three categories, where each has a specific pattern and timing:
- Early: these decelerations are usually characterized by a drop in the baby’s heart rate aligning with the mother’s uterine contractions. So, when the contraction ends, the heart rate of the baby also recovers.
- Late: the baby’s heart rate usually falls after the mother’s contractions end.
- Variable: these happen irrespective of the mother’s uterine contractions. In this case, the decrease in the baby’s heart rate lasts for at least 15 seconds before recovery.
Decelerations are labeled as recurrent if they happen in more than 50 percent of the mother’s uterine contractions within a 20-minute period.
Track your symptoms with Femia and get tailored
health advice right on your phone
What causes late decelerations?
One of the main reasons for late recurrent decelerations are contractions. That is because contractions put pressure on the uterine walls, making it harder for blood flow to reach the placenta – so, the fetus cannot get enough blood and oxygen for their heart rate to be normal.
While contractions are the most common cause, there are some conditions that may lead to late decels:
- Maternal anemia or dehydration;
- Hypotension caused by an epidural;
- Reduced placental exchange between the the fetus and placenta;
- Hypoxia;
- Hypertensive disorders, diabetes, and IUGR;
- Uterine tachysystole.
Significance of late decelerations during labor
Late fetal decelerations usually alert the medical team that the baby may experience a lack of oxygen or decreased blood flow to the placenta.
Late decelerations are very concerning, especially if they become recurrent. Your medical team will first evaluate when the deceleration begins and ends, checking if it aligns with maternal contractions. If decelerations are late and occur with more than 50 percent of the mother’s contractions over 20 minutes, doctors will diagnose fetal distress.
Then, the team will evaluate the severity of the decelerations. This happens by checking whether other decelerations are present, including early and variable ones. The absence of other decelerations means impaired blood flow to the placenta.
This greatly reduces the amount of nutrients and oxygen the fetus gets. Babies suffering from late decelerations may be born with low APGAR scores.
The APGAR is a widely used scoring system that evaluates a baby’s overall health after birth. The system tests muscle tone, heart rate, appearance, response, and respiration on a scale of zero to 10. Any score of 7 or above is considered a good one, so those babies with score below 7 may need additional intervention and are usually transferred to intensive care.
The worst case scenario here, when decelerations are not properly treated by the medical team, is fetal hypoxia and metabolic acidosis – a buildup of acid in the baby’s blood.
Do late decelerations have long-term complications?
If late decels are not handled or persist even after treatment, they might have long-term complications for the baby.
Late recurrent decelerations decrease the baby’s placental blood flow and oxygen supply. This may increase the risk of mild and severe brain damage in a baby. This, in turn, might cause hypoxic-ischemic encephalopathy, or HIE, and cerebral palsy.
Timely diagnosis and medical intervention are required to prevent any of these long-term complications.
What are nursing interventions in the case of late decelerations?
How doctors manage and treat recurrent late decelerations depends on their cause and the time they begin. The key goal is to redirect the blood to the placenta so the baby’s heart rate returns to normal until they are born. So, the interventions for late decelerations strive to increase the baby’s oxygen levels as soon as possible to prevent potential complications.
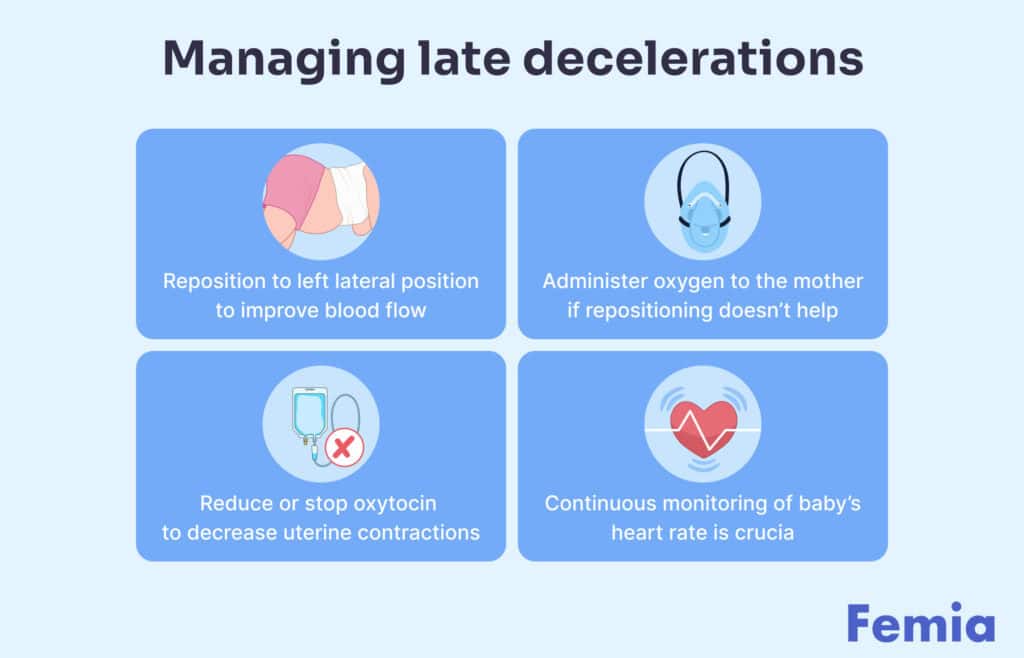
Here are the main nursing interventions for late decelerations:
1. Repositioning the mother to improve blood flow (e.g., left lateral position)
A baby’s blood circulation can be influenced by changing the mother’s position.
Putting the mother into the left lateral position, preferably with the knees bent towards the chest, is often the first step to reduce excess uterine pressure and improve placental blood flow. Nurses should continuously monitor the baby’s heart rate during repositioning to ensure late decelerations end.
2. Administering oxygen to the mother
If the first step does not return the baby’s heart rate to normal, nurses may also want to administer oxygen. There is no evidence that maternal O2 administration improves the baby’s heart rate, though supplemental oxygen is still a standard practice when a baby’s heart abnormality remains.
3. Reducing or stopping oxytocin if it's being used
There is no one opinion on the ideal dosing regimen of oxytocin. However, one study found that induction with higher dose oxytocin increments is often associated with an increase in uterine hyperstimulation, while low dose oxytocin is proven to be safe for labor induction.
So, stopping or at least reducing oxytocin labels may also be considered to prevent late decels. Continuous monitoring of the baby’s heart rate should still be applied to verify nurses’ decisions.
4. Assessing and treating maternal hypotension if present
Hypotension may occur as a result of epidural anesthesia. If this happens and affects the baby’s heart rate, it can be managed by giving the mother an intravenous fluid bolus or by alpha-adrenergic agonists prescribed and inserted by the anesthesiologist.
What are treatment options for late decelerations?
If nursing interventions are unsuccessful and the baby’s heart rate remains abnormal, the risk of both short- and long-term complications increases.
In these cases, the following treatment for late decelerations might be available:
Track your symptoms with Femia and get tailored
health advice right on your phone
1. Reduce uterine contractions
If the gynecologist thinks that uterotonic medication is increasing the contractions, they may consider discontinuing administration. This should help relax the uterine muscles over time and allow blood flow to return to the baby.
In case of uterine contractions being the cause of late decelerations, doctors may also want to administer tocolytics, such as terbutaline, to reduce the frequency of uterine contractions. This medication may help relax the uterine muscles and thereby improve placental perfusion in the fetus.
2. Intravenous fluid administration
Other treatments might be necessary depending on what causes the late recurrent decelerations. If an epidural results in hypotension, doctors may want to consider administering intravenous fluids. Intravenous administration means “via a vein” – giving fluids through a needle or tube inserted into a vein to ease the mother’s hypotension and increase blood flow to the placenta.
3. Immediate vaginal delivery or Cesarean section
If any of the above-mentioned conservative options do not return the baby’s heart rate to normal, the last two steps doctors should take to prevent complications are either immediate vaginal delivery or a Cesarean section (C-section).
Questions from the Femia community
Are late decelerations ever a normal part of labor?
The short answer is “no.” If late decelerations occur, they are a sign the baby is not getting enough oxygen. A baby's heart rate should always be carefully monitored throughout labor to ensure everything goes smoothly. Anytype of deceleration, especially late recurring ones, means your healthcare team should immediately take action to bring the baby's heart rate back to normal.
How do doctors find out about late decelerations?
Fetal heart rate is an essential factor indicating how a baby is feeling during the labor, so close monitoring is a common practice. Doctors use electronic monitors to keep track of the baby's heart rate, allowing them to quickly spot any abnormalities.
Can drinking water help with late decelerations?
Staying hydrated during labor is always a good idea, though late decelerations aren't linked to a mother's hydration – they are more about how oxygen and blood are delivered to the placenta.
Will I need extra tests if late decelerations show up?
Sometimes, your doctors may want to do other tests like an ultrasound to check the baby's wellbeing.
Does having late decelerations mean I'll need a C-section?
No, not always. In most cases, late decelerations can be managed by changing the mother's position, administering supplemental oxygen, and reducing the frequency of contractions. However, if they continue, an immediate vaginal delivery (when possible) or C-section are usually the safest options.
What can I do to help if there are late decelerations?
It is important to stay calm, follow your healthcare team's advice while they try to manage the decelerations.
Are certain health conditions in moms linked to late decelerations?
While late decelerations are usually caused by contractions, conditions like high blood pressure, diabetes, or preeclampsia may also increase the risk of late decels in labor.
The bottom line
Late decelerations mostly happen because of contractions. Your medical team will keep a close eye on the fetal heart rate to quickly identify late decelerations and try to manage them by changing your position, administering oxygen, and reducing the frequency of contractions. When properly handled, doctors can treat late decelerations, prevent any long-term complications, and keep you and your baby safe during and after labor.
References
- Sholapurkar, Shashikant L. “Categorization of Fetal Heart Rate Decelerations in American and European Practice: Importance and Imperative of Avoiding Framing and Confirmation Biases.” Journal of Clinical Medicine Research, vol. 7, no. 9, 2015, pp. 672–680, https://doi.org/10.14740/jocmr2166w.
- “Recurrent Deceleration (Concept Id: C2985322) – MedGen – NCBI.” Www.ncbi.nlm.nih.gov, www.ncbi.nlm.nih.gov/medgen/457548. Accessed 29 May 2024.
- Pillarisetty, Leela Sharath, and Bradley N. Bragg. “Late Decelerations.” PubMed, StatPearls Publishing, 2022, www.ncbi.nlm.nih.gov/books/NBK539820/#:~:text=The%20central%20pathophysiology%20behind%20late.
- Leela Sharath Pillarisetty, and Bradley N Bragg. “Late Decelerations.” Nih.gov, StatPearls Publishing, 4 June 2019, www.ncbi.nlm.nih.gov/books/NBK539820/.
- “Recurrent Deceleration (Concept Id: C2985322) – MedGen – NCBI.” Www.ncbi.nlm.nih.gov, www.ncbi.nlm.nih.gov/medgen/457548. Accessed 29 May 2024.
- Simon, Leslie V., et al. “APGAR Score.” PubMed, StatPearls Publishing, 22 May 2023, www.ncbi.nlm.nih.gov/books/NBK470569/.
- Graham, Ernest M., et al. “Diagnostic Accuracy of Fetal Heart Rate Monitoring in the Identification of Neonatal Encephalopathy.” Obstetrics & Gynecology, vol. 124, no. 3, Sept. 2014, pp. 507–513, https://doi.org/10.1097/aog.0000000000000424. Accessed 5 Dec. 2022.
- Jani, Devanshi, et al. “The Effect of Maternal Position on Placental Blood Flow and Fetoplacental Oxygenation in Late Gestation Fetal Growth Restriction: A Magnetic Resonance Imaging Study.” The Journal of Physiology, 19 July 2023, https://doi.org/10.1113/jp284269. Accessed 2 Nov. 2023.
- Chopra, Seema, et al. “Stopping Oxytocin in Active Labor rather than Continuing It until Delivery: A Viable Option for the Induction of Labor.” Oman Medical Journal, vol. 30, no. 5, 15 Sept. 2015, pp. 320–325, https://doi.org/10.5001/omj.2015.66. Accessed 17 Nov. 2020.
- Pillarisetty, Leela Sharath, and Bradley N. Bragg. “Late Decelerations.” PubMed, StatPearls Publishing, 2024, www.ncbi.nlm.nih.gov/books/NBK539820/#:~:text=Intravenous%20hydration%3A%20hypotension%20secondary%20to. Accessed 29 May 2024.
- Schifrin, Barry S., et al. “Approaches to Preventing Intrapartum Fetal Injury.” Frontiers in Pediatrics, vol. 10, 23 Sept. 2022, www.ncbi.nlm.nih.gov/pmc/articles/PMC9537758/, https://doi.org/10.3389/fped.2022.915344.
- Petrie, R. H., and P. Danilo. “Maternal and Fetal Effects of Uterine Stimulants and Relaxants.” Diagnostic Gynecology and Obstetrics, vol. 3, no. 2, 1981, pp. 111–117, pubmed.ncbi.nlm.nih.gov/6114825/. Accessed 29 May 2024.
- Holte, Kathrine, et al. “Epidural Anesthesia, Hypotension, and Changes in Intravascular Volume.” Anesthesiology, vol. 100, no. 2, Feb. 2004, pp. 281–286, https://doi.org/10.1097/00000542-200402000-00016. Accessed 5 Apr. 2020.
- Velayudhareddy, S, and H Kirankumar. “Management of Foetal Asphyxia by Intrauterine Foetal Resuscitation.” Indian Journal of Anaesthesia, vol. 54, no. 5, 2010, p. 394, https://doi.org/10.4103/0019-5049.71032.

Postpartum supplements are packed with much-needed vitamins for recovery and milk production after pregnancy. Here is how to choose the best postnatal vitamins.

Struggling with the 8-month sleep regression? Learn why it happens, common signs, and expert tips to help your baby sleep better.

Discover the complete guide on how to get pregnant fast, including the methods and tips for faster conception, nutrition and supplements, intercourse timings and more.