Femia > Health Library > Pregnancy > Pregnancy health > Down syndrome ultrasound vs normal: What is the difference?
Down syndrome ultrasound vs normal: What is the difference?

- Updated Mar 2, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
Ultrasounds can help screen for Down syndrome, but can’t provide a definitive diagnosis:
- Key ultrasound markers include increased nuchal translucency, absent nasal bone, shortened thigh bone, and certain heart or bowel abnormalities.
- These markers only indicate increased risk, not a confirmed diagnosis.
- Additional diagnostic tests like NIPT, amniocentesis, or CVS are needed for a definitive diagnosis.
- Many babies with concerning ultrasound markers are born without Down syndrome. Only genetic testing can confirm Down syndrome.
Back in the day, soon-to-be mamas could only pray for the health of their babies. Now, modern medicine has taken the guessing out of the equation.
Ultrasound scans can provide valuable information about your baby’s growth and development. They may show certain physical markers that could indicate an increased risk of chromosomal conditions.
Ultrasounds are a key and well-known part of prenatal care. In fact, you likely already have a good idea of what an ultrasound, also known as sonography, looks like—just think of all the movies that show pregnant women seeing their babies for the first time. It is an exciting event, but always a bit nerve-wracking. So, as you lay on the table and carefully analyze your healthcare provider’s every facial expression, remember to breathe and relax.
Before we compare a Down syndrome ultrasound vs normal scan, let’s discuss how conditions like this might be noticed and diagnosed during each stage of pregnancy.

Finding out if your baby has Down syndrome—at each stage of pregnancy
Checking whether your baby has Down syndrome is a thorough process. You will likely go through multiple tests to get more clarity and confirm the diagnosis. However, the process is different in each semester.
First trimester
To check for risk signs (screening), you will be offered an ultrasound and blood test. An ultrasound will check for signs of Down syndrome, while the blood test will look for specific markers, like proteins, that indicate an increased risk of your baby having Down syndrome.
If initial screening tests suggest a higher risk, your healthcare provider may offer additional diagnostic testing for more definitive information. These tests analyze your baby’s genetic material, including chromosome 21, which is associated with Down syndrome.
One such test is chorionic villus sampling (CVS). Here’s what you need to know:
- According to the American College of Obstetricians and Gynecologists (ACOG), CVS is typically performed between 10 and 13 weeks of pregnancy. This timeframe allows for the safest and most accurate results.
- The procedure involves collecting a small sample of cells from the placenta.
- Results are usually available within 1-2 weeks after the test.
- It’s important to remember that CVS is a diagnostic test, meaning it can provide a definitive answer about certain chromosomal conditions. However, like all medical procedures, it comes with both benefits and risks.
Second trimester
For screening, you can get an ultrasound and a blood test. There is also a combined method that uses both a blood test and an ultrasound during the first trimester, as well as a second-trimester blood test. Healthcare providers then combine all these results to produce one Down syndrome risk rating.
For making the diagnosis, most parents are offered amniocentesis (usually done between weeks 15 and 20). You could also have percutaneous umbilical blood sampling (PUBS), done after week 18.
Since diagnostic tests rely on analyzing genetic material, they are more invasive than screening methods, and there is a slight risk of triggering a miscarriage. If you and your family are considering prenatal diagnostic testing for Down syndrome, discuss all the risks and benefits with your trusted healthcare provider.
👉Find out more: Your pregnancy checklist: Week-by-week guide to preparing for baby
What is an ultrasound, and how does it work?
Ultrasound imaging is a prenatal screening method that uses high-frequency sound waves to create real-time images of your baby in the womb. As a non-invasive, painless, and overall safe intervention, you can have it several times without worrying about affecting your baby’s health.
Why is ultrasound imaging such an important part of pregnancy care? It can be used in so many ways: to assess the gestational age, monitor the baby’s growth, and detect potential anomalies (such as defects in the brain, heart, or limbs). Ultrasounds also tell us the number of babies and the position of the placenta (an organ that connects you and your baby), as well as help guide interventions like amniocentesis.
In most cases, ultrasound exams are performed by sonographers. You will be asked to lie on your back and reveal your baby bump. The sonographer will apply gel on your tummy and place a probe over it. As the probe is moved, pictures of your baby from different angles will appear on the screen. The sonographer might have to apply slight pressure to get a good view of the baby, but the intervention should not be painful.
You will likely have at least two ultrasound scans during pregnancy: the 12-week ultrasound and 20-week ultrasound.
Normal ultrasound findings
At your 12-week ultrasound, your healthcare provider will be looking at several important factors:
- Confirming your due date. The sonographer will measure your baby’s crown-rump length (CRL), which should be about 5-6 cm at this stage. This helps accurately date your pregnancy.
- Assessing risk for chromosomal abnormalities. This is a crucial part of the 12-week scan. The provider will:
- Measure the nuchal translucency (NT), which is a fluid-filled space at the back of your baby’s neck. This measurement is key in screening for conditions like Down syndrome.
- Check for the presence of the nasal bone, another important marker.
- Examining basic anatomy. While your baby is still tiny, the major structures like the brain, heart, and limbs are beginning to form. The sonographer will check these developing organs.
The 20-week ultrasound is also known as the anatomy scan. By this time, your baby will have grown significantly. The typical CRL at 20 weeks is 16–20 cm, and the weight should be around 300 grams.
Your sonographer will make sure that the brain and heart structures are all without defects. The spine, kidneys, bladder, stomach, and limbs are also visualized to ensure proper formation. To check for abnormalities and developmental concerns, your sonographer will also make sure that the thigh bone (femur) of your baby is the correct length, as well as the head circumference.
Down syndrome ultrasound signs
An ultrasound can tell a lot about your baby’s health and even suggest a potential health condition. Let’s explore the signs of Down syndrome during pregnancy ultrasound testing.
What does a positive Down syndrome ultrasound look like? This is what your provider will be looking for.
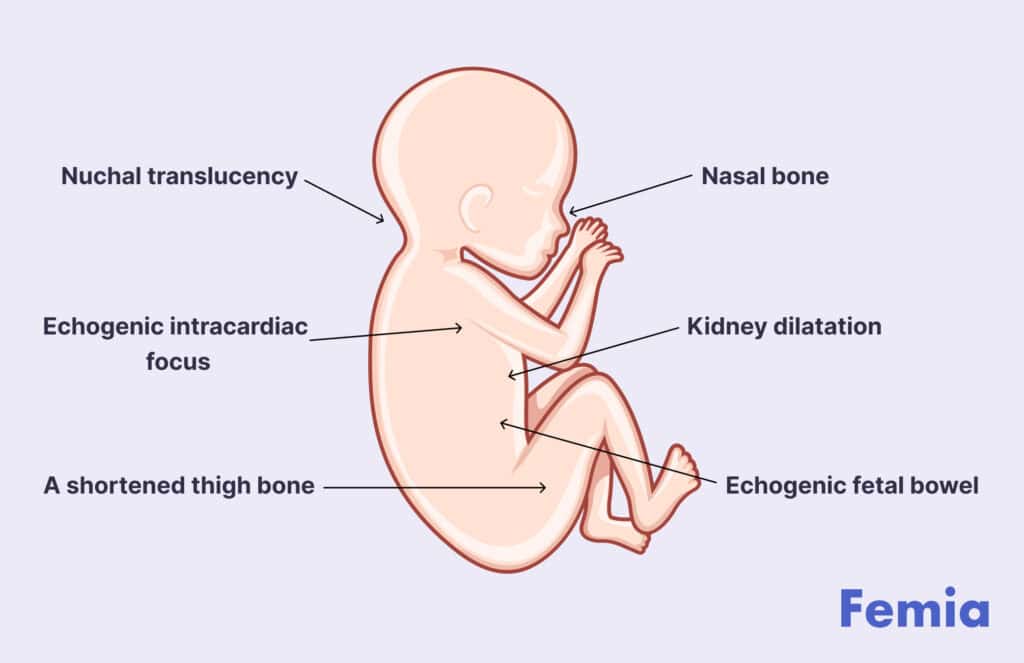
1. Nuchal translucency. Increased thickness in the fluid at the back of the baby’s neck, measured during the 11–14 week scan, might suggest an increased risk of Down syndrome.
Important note: An increased NT measurement may suggest a higher risk of chromosomal conditions, including Down syndrome. However, it’s important to understand that:
- This is a screening tool, not a diagnostic test.
- Many babies with increased NT measurements are born perfectly healthy.
- If the NT is increased, your provider will discuss further options with you, which may include additional screening or diagnostic tests.
2. Nasal bone. How does the nasal bone look in a Down syndrome ultrasound vs normal ultrasound? With Down syndrome, the nasal bone might be smaller in size or completely absent. In some cases, a smaller or hard-to-see nasal bone might be associated with an increased chance of Down syndrome. However, it’s important to remember that this is just one piece of the puzzle. Many babies with small or hard-to-see nasal bones at this stage are born perfectly healthy.
3. A shortened thigh bone. The baby’s thigh bone, also known as the femur, not matching the standard for gestational age might be an indicator of Down syndrome.
4. Kidney dilatation. A renal pelvis wider than normal (over 4 mm) is also known as pyelectasis. This marker is not very specific but can increase risk when interpreted along with other signs.
5. Echogenic intracardiac focus. Babies positive for Down syndrome often have a bright spot in the heart area seen during the 20-week scan.
6. Echogenic fetal bowel. If the bowel of your baby appears very bright on screen, that might indicate an increased risk of Down syndrome.
Normal vs. abnormal 12-week and 20-week ultrasounds
What abnormalities can be seen at 12-week scan that are normally not there? On a normal ultrasound, the CRL and nuchal translucency are standard length, with nuchal fluid typically below 3 mm. The nasal bone and other developing structures, such as the brain, heart, and limbs, should be forming properly.
The difference between a normal vs abnormal 12 week ultrasound is very subtle, since the baby is just starting to develop. With an abnormal ultrasound, the first signs your sonographer notices might be a nuchal translucency and CRL are larger than the expected range. The nasal bone might be deformed or completely absent, and there might be abnormalities with the major organs—deformities, missing parts, or absence.
Now, let’s compare how things look with Down syndrome ultrasound vs normal 20 weeks ultrasound. A normal scan would show well-formed brain structures, a properly functioning four-chambered heart, and standard-length limbs.
At this stage, markers that could raise concerns for Down syndrome include shorter-than-average thigh bone length, bright spots in the heart, or certain brain abnormalities like enlarged inner cavities or ventricles.
If your sonographer notices a high-risk marker, try your best to stay calm. Remember that these signs appear in many healthy pregnancies and cannot be used to diagnose Down syndrome. If multiple markers are observed, further diagnostic testing, such as amniocentesis, may be recommended to provide a more accurate assessment.
👉Find out more: Getting a Pap smear during pregnancy: safety, timing, and what to expect
What happens after an abnormal ultrasound finding?
Most prenatal screening tests will not find anything wrong, but there’s a chance you’ll be told that your baby could be born with a genetic condition. Remember that screening methods (ultrasound and blood tests) cannot be used to diagnose Down syndrome, but they do point out high-risk cases. So, what comes next? You will be offered diagnostic tests to confirm or rule out the diagnosis.
Non-invasive prenatal testing
Non-invasive prenatal testing (NIPT) relies on using a sample of your blood . As your blood carries your baby’s DNA (genetic material), this test might be able to detect if your baby has an extra chromosome 21, which causes Down syndrome.
Amniocentesis
Amniocentesis involves taking a small sample of cells from the amniotic fluid surrounding your baby in the uterus. The genetic material from these cells is then analyzed to confirm the diagnosis.
Your healthcare provider would insert a very thin needle into your belly and guide it with an ultrasound to only penetrate the amniotic sac. The test usually takes about 30 minutes. Most women describe it as uncomfortable, rather than painful.
Amniocentesis is usually performed between 15 and 20 weeks gestation, but it can be done later if needed. An amniocentesis performed before week 15 is referred to as an “early” amniocentesis. It might increase the risk of complications (like miscarriage), so it is usually avoided.
Chorionic villus sampling
Chorionic villus sampling (CVS) involves taking a small sample of cells from the placenta, the organ linking you and your unborn baby. The genetic material from the cells is then analyzed to confirm the diagnosis.
CVS can be done in a similar way as amniocentesis, by inserting a thin needle to your tummy. This is the most common method used; however, it can also be done by inserting a smooth metal instrument through the vagina and cervix. The test usually takes about 30 minutes and might be a bit uncomfortable rather than painful. You might experience some cramps, similar to period pains, for a few hours afterward.
Unlike amniocentesis, CVS is not routinely performed in pregnancy. When it is done, it will happen between weeks 11 and 14, but it can also be performed later if needed.
Understanding the emotional impact
Finding out that your baby might have a genetic condition is hard. The whole diagnostic process can be nerve-wracking and excruciating at times. When you feel like nothing is in your control, know that there is always support available.
Your primary source of comfort might be your partner, family, or friends. However, sometimes support from outside your circle might be just what you need. Check if there are local support groups in your area, charities that support families with your baby’s potential condition, or counselors that specialize in helping parents cope with their baby’s health concerns.

Questions from Femia community
Can my baby receive a final diagnosis of Down syndrome based on an ultrasound?
No, ultrasound imaging cannot definitively diagnose Down syndrome. It is just a screening method for chromosomal abnormalities—-it can point out markers that indicate an increased risk of your baby having a condition. You and your baby will have to undergo further diagnostic tests like amniocentesis or CVS to confirm a Down syndrome diagnosis.
Can I trust the accuracy of ultrasound markers in detecting Down syndrome?
Ultrasound markers are considered screening tools that can only detect an increased risk of your baby having Down syndrome. But, that is not a conclusive sign of a health condition. Many pregnancies with concerning ultrasound markers result in healthy babies without Down syndrome.
Am I at risk for complications if I get follow-up diagnostic tests after an abnormal ultrasound?
Yes, diagnostic tests like amniocentesis and CVS are invasive and carry a small risk of miscarriage. Before you go through with testing, talk about the risks and benefits with your trusted healthcare provider.
The bottom line
Ultrasounds have played a huge part in modern medical diagnostics. They can tell us a lot about your baby’s progress and potential health concerns. However, ultrasound imaging is not 100% accurate and can only suggest that something is wrong. Sometimes, that is not the case, and the baby will be born completely healthy.
If your ultrasound exam has not gone as well as you hoped, try to calm down and wait for the results of more accurate diagnostic tests like NIPT or amniocentesis. Remember, only these diagnostic tests can confirm whether your baby has Down syndrome based on DNA analysis. This is the reality of many soon-to-be parents and, as painful it may be, it is always best to know if something is wrong in advance.
References
- “Amniocentesis.” National Health Service (NHS), 20 Oct. 2017, https://www.nhs.uk/conditions/amniocentesis/.
- Bethune, Michael, et al. “A Pictorial Guide for the Second Trimester Ultrasound.” Australasian Journal of Ultrasound in Medicine, vol. 16, no. 3, Aug. 2013, pp. 98–113. PubMed Central, https://doi.org/10.1002/j.2205-0140.2013.tb00106.x.
- “Chorionic Villus Sampling.” National Health Service (NHS), 7 June 2018, https://www.nhs.uk/conditions/chorionic-villus-sampling-cvs/.
- Gaillard, Frank. “Echogenic Fetal Bowel.” Radiopaedia, https://doi.org/10.53347/rID-1256. Accessed 13 Aug. 2024.
- “How Do Health Care Providers Diagnose Down Syndrome? | NICHD – Eunice Kennedy Shriver National Institute of Child Health and Human Development.” NIH, https://www.nichd.nih.gov/health/topics/down/conditioninfo/diagnosis. Accessed 11 Aug. 2024.
- Kazemi, Mohammad, et al. “Down Syndrome: Current Status, Challenges and Future Perspectives.” International Journal of Molecular and Cellular Medicine, vol. 5, no. 3, 2016, pp. 125–33.
- Olney, Richard, et al. “Chorionic Villus Sampling and Amniocentesis: Recommendations for Prenatal Counseling.” CDC, https://www.cdc.gov/mmwr/preview/mmwrhtml/00038393.htm. Accessed 13 Aug. 2024.
- Souka, Athena P., et al. “Screening for Major Structural Abnormalities at the 11- to 14-Week Ultrasound Scan.” American Journal of Obstetrics and Gynecology, vol. 194, no. 2, Feb. 2006, pp. 393–96. ScienceDirect, https://doi.org/10.1016/j.ajog.2005.08.032.
- Ulrich, Cayla C., and Olga Dewald. “Pregnancy Ultrasound Evaluation.” StatPearls, StatPearls Publishing, 2024. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK557572/.
- “Ultrasound Scans in Pregnancy.” National Health Service (NHS), 3 Dec. 2020, https://www.nhs.uk/pregnancy/your-pregnancy-care/ultrasound-scans/.
- Weerakkody, Yuranga. “Echogenic Intracardiac Focus.” Radiopaedia, https://doi.org/10.53347/rID-10787. Accessed 13 Aug. 2024.
- “Shortened Fetal Femur.” Radiopaedia, https://doi.org/10.53347/rID-13481. Accessed 13 Aug. 2024.

Get 1 to 3-month pregnancy diet chart and first trimester meal plan from expert. Explore the best pregnancy food chart with essential nutrients for your and baby health.

Learn how ovulation and implantation cramps differ in timing, spotting and pain.

Struggling to conceive? Common reasons such as PCOS, lifestyle factors or age might be contributing. Get insights into what you can do and when to seek medical advice.

