Femia > Health Library > Pregnancy > Pregnancy health > Positive pregnancy test but no baby on ultrasound: What could it mean?
Positive pregnancy test but no baby on ultrasound: What could it mean?
- Updated Mar 1, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
- Not seeing a baby on your ultrasound after a positive pregnancy test does not always mean you are not pregnant. The embryo may be too small to see before 5-6 weeks.
- Other reasons may include blighted ovum (anembryonic pregnancy), ectopic pregnancy, and miscarriage.
- Follow your doctor’s advice for follow-up tests. Usually, waiting 1-2 weeks and repeating the ultrasound resolves uncertainty.
Receiving a positive result on a pregnancy test may come with different emotions for everyone. However, the follow-up ultrasound showing no signs of pregnancy definitely causes confusion and distress.
A pregnancy test works by identifying the presence of the hormone human chorionic gonadotropin (hCG), which your body produces during pregnancy. It’s common for women to expect this sign to be confirmed by an ultrasound. However, there are several reasons why a scan may not show a baby even if the test is positive.
We’ve created this guide to help you learn the most common reasons for a positive pregnancy test but no baby on ultrasound and what to expect next.
👉Find out more: Can you get pregnant after your period? Understanding your fertility window

Understanding early pregnancy and ultrasound timing
A positive pregnancy test result indicates the presence of hCG in your body. This hormone is produced once a fertilized egg attaches to the uterine lining and is one of the key signs of pregnancy.
However, in some cases, there could be high hCG levels but no baby on ultrasound. While this often causes distress and worry, there are medical reasons why this might happen. Often, that reason is just the early stages of pregnancy.
At the very beginning of your pregnancy journey (from 1–5 weeks), it’s possible for the embryo to be too small to be seen. In some cases, the pregnancy has not progressed enough for an ultrasound to detect an embryo.
An ultrasound done too early in the pregnancy may not be able to visualize the tiny gestational sac (a fluid-filled structure that surrounds the embryo during the first few weeks of development) or developing embryo—it’s pretty common.
👉Find out more: Is it normal to not feel pregnant? Understanding early pregnancy and what to expect
When is a gestational sac visible?
In most cases, an ultrasound can show a gestational sac by weeks five to six of the pregnancy. By the sixth week, the scan may also detect a yolk sac (a structure developing inside the gestational sac during early pregnancy) or even the beginnings of a fetal pole (the first stage of an embryo’s development).
Timing plays a crucial role in what an ultrasound will detect, and this relies on several factors. These include the exact timing of ovulation and conception, as well as the accuracy of the pregnancy dating. So, if ovulation occurred later than you expected it or if the pregnancy is younger than initially calculated, the gestational sac might not yet be visible, even at five weeks.
The yolk sac is usually visible by the sixth week; however, the baby (embryo) and its heartbeat may still not be detectable. If this is the case, or the gestational sac itself isn’t visible yet, your healthcare provider may recommend waiting for another two weeks and repeating the test. This wait often resolves the uncertainty, as the pregnancy may just be at its very beginning.
Other possible reasons for no baby on ultrasound
Contrary to common belief, a negative ultrasound with a positive test is a pretty common case, especially when it comes to the early weeks of a pregnancy. Aside from being too early in the pregnancy for an embryo to be visible, there are several potential reasons why you cannot see a fetus on an ultrasound.
1. Blighted ovum
When a fertilized egg implants in the uterus, it may result in a blighted ovum, also called an anembryonic pregnancy. In this case, a gestational sac forms, but the embryo does not develop. This condition is a common reason for early pregnancy loss and might be detected during an ultrasound when the sac is seen but there is no embryo in it.
2. Ectopic pregnancy
An ectopic pregnancy is a term used for when an embryo implants outside the uterus, often in the fallopian tube. Simply put, the embryo is not where it is supposed to be, so ultrasound won’t detect it even with a positive pregnancy test. Aside from a lack of embryo in the uterus, signs of an ectopic pregnancy include indicators like fluid in the pelvis. This condition requires urgent medical attention.
3. Miscarriage
The last reason for an ultrasound with no baby is early miscarriage. Even after a miscarriage occurs, the levels of hCG in your body may remain elevated for some time, causing confusion. In these cases, the gestational sac may be seen, but there won’t be an embryo, indicating that there has been a miscarriage.
👉Find out more: Period vs. miscarriage: How to tell the difference
What causes hCG levels to rise if not pregnant?
The hCG hormone is usually associated with pregnancy, since it is produced by the placenta once a fertilized egg implants in the uterus. However, hCG levels can rise even in the case when a woman isn’t pregnant due to a variety of medical conditions or testing errors.
Medical conditions that cause hCG levels to rise:
- Ectopic pregnancy. When a fertilized egg implants outside the uterus, called an ectopic pregnancy, it can cause increased HCG levels despite the absence of a viable pregnancy.
- Trophoblastic diseases. Hydatidiform mole (a type of gestational trophoblastic disease) is a condition that causes the abnormal growth of cells that usually develop into a placenta. This may confuse the body and cause significantly elevated hCG levels.
- Pituitary hCG secretion. The pituitary gland (located at the base of your brain) normally produces low hCG levels. However, in some cases, sensitive pregnancy tests may detect these hormones in the blood or urine.
- Certain types of cancers. It’s rare, but some cancers, such as choriocarcinoma (one that occurs in the uterus) and certain ovarian or testicular cancers can also produce high hCG levels.
- HCG-secreting tumors. There are some tumors that don’t relate to pregnancy but sometimes secret hCG. These may be located in the lungs, kidney, or gastrointestinal tract.
Errors in testings:
- Laboratory errors. Even with a high level of precision, sometimes laboratory blood tests can lead to false positive results. This may happen because of improper sample handling, contamination, or cross-reactivity with other substances in your blood.
- Biotin interference. Consuming high doses of biotin (a popular supplement for hair, skin, and nail health) may interfere with certain immunoassay tests, leading to increased hCG levels.
- Heterophile antibodies. In rare cases, women may have antibodies that have been shown to interfere with the hCG test, causing a falsepositive result. So, antibodies may mimic the presence of hCG.
Follow-up steps: What to do next
We understand how stressful it could be to hear that doctors are not sure about your pregnancy, and it’s even more stressful to wait a few weeks before they can confirm a result.
It’s important to ask all the questions you may have, and seek professional support to resolve any myths and worries. In the majority of cases, your healthcare provider will recommend a follow-up ultrasound and blood test to monitor hCG levels.
It’s vital to follow the guidelines prescribed by your doctor, as this will be the only way to determine the cause of not seeing a baby on your scans. You may want to repeat the ultrasound a week or two later, but it’s always best to get personalized recommendations and follow them as precisely as possible, so your doctors can determine the next steps in your specific case.
Emotional considerations and support
It can be emotionally challenging to have a positive pregnancy test but no baby on scan, and even more so having to wait two weeks for a follow-up ultrasound. Taking care of your emotional health is essential to overcome the stressful situation and patiently wait.
That’s why we highly recommend seeking emotional support—whether it’s from your healthcare provider, with more information to reduce your stress; your partner, to help you distract while you wait; or friends and family, to help you feel taken care of.
Ask for help, seek support groups, discuss your worries with your loved ones, and make sure you consider your feelings in this distressing time.

Questions from the Femia community
Can a tilted uterus affect what's seen on my early ultrasound?
The short answer is yes. A retroverted uterus may create more pressure on your bladder, especially during the first trimester. This may lead to a positive pregnancy test but no gestational sac being visible until the uterus begins to enlarge with pregnancy.
Is it possible for twins to cause one baby to be missed on an ultrasound?
Although it is rather rare, ultrasounds before eight weeks might miss one twin, especially if it is obscured by the other. If your results are unclear, a healthcare provider may recommend waiting for a few weeks to reveal your multiple pregnancy more clearly.
What should I do if I'm experiencing pain along with a positive test but no baby on the ultrasound?
Pain and heavy bleeding are signs that you need urgent medical help. These could mean that you have ectopic pregnancy, miscarriage, or other complications.
The bottom line
If you have a positive pregnancy test but nothing on ultrasound, it’s important to remain calm and seek timely medical evaluation. There are several reasons for this to happen, ranging from simply being too early in the pregnancy to conditions like a blighted ovum, ectopic pregnancy, or miscarriage.
While this can be confusing and stressful, know that many cases are resolved with follow-up care, and your healthcare provider is there to guide you through each step. Don’t hesitate to ask questions and seek support as you navigate this uncertain time.
References
- Barnhart, Kurt T. “Early Pregnancy Failure: Beware of the Pitfalls of Modern Management.” Fertility and Sterility, vol. 98, no. 5, Nov. 2012, pp. 1061–1065, https://doi.org/10.1016/j.fertnstert.2012.09.018.
- Wikipedia Contributors. “Gestational Sac.” Wikipedia, Wikimedia Foundation, 14 Feb. 2024, en.wikipedia.org/wiki/Gestational_sac. Accessed 21 Aug. 2024.
- Dewald, Olga, and Jennifer T. Hoffman. “Gestational Sac Evaluation.” PubMed, StatPearls Publishing, 2023, www.ncbi.nlm.nih.gov/books/NBK551624/#:~:text=The%20gestational%20sac%20is%20the.
- “Yolk Sac in Early Pregnancy: Meaning & Function.” Cleveland Clinic, my.clevelandclinic.org/health/body/22341-yolk-sac.
- Wikipedia Contributors. “Human Chorionic Gonadotropin.” Wikipedia, Wikimedia Foundation, 17 Feb. 2019, en.wikipedia.org/wiki/Human_chorionic_gonadotropin.
- “Blighted Ovum: What Causes It?” Mayo Clinic, 2016, www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/expert-answers/blighted-ovum/faq-20057783.
- Mayo Clinic. “Ectopic Pregnancy – Symptoms and Causes.” Mayo Clinic, Mayo Clinic, 12 Mar. 2022, www.mayoclinic.org/diseases-conditions/ectopic-pregnancy/symptoms-causes/syc-20372088.
- “Missed Miscarriage.” The Miscarriage Association, www.miscarriageassociation.org.uk/information/miscarriage/missed-miscarriage/.
- Murray, Heather. “Diagnosis and Treatment of Ectopic Pregnancy.” Canadian Medical Association Journal, vol. 173, no. 8, 11 Oct. 2005, pp. 905–912, www.ncbi.nlm.nih.gov/pmc/articles/PMC1247706/, https://doi.org/10.1503/cmaj.050222.
- “Molar Pregnancy.” Wikipedia, 20 July 2022, en.wikipedia.org/wiki/Molar_pregnancy.
- “Human Chorionic Gonadotropin.” Wikipedia, 14 Jan. 2024, en.wikipedia.org/wiki/Human_chorionic_gonadotropin#:~:text=The%20pituitary%20analog%20of%20hCG.
- Canadian Cancer Society / Société canadienne du. “Human Chorionic Gonadotropin (HCG or B-HCG).” Canadian Cancer Society, cancer.ca/en/treatments/tests-and-procedures/human-chorionic-gonadotropin-hcg-or-b-hcg#:~:text=If%20you%20have%20liver%2C%20stomach.
- Mustafa, Aynur, et al. “An Unexpected Reason for Elevated Human Chorionic Gonadotropin in a Young Woman. Cervical Squamous Carcinoma.” Saudi Medical Journal, vol. 37, no. 8, 27 Aug. 2016, pp. 905–907, https://doi.org/10.15537/smj.2016.8.14529.
- Sobolevsky, Tim, and Brian Ahrens. “Biotin as a Masking Agent in Chorionic Gonadotropin Assays Utilizing Biotinylated Antibodies.” Drug Testing and Analysis, vol. 13, no. 11-12, 1 Nov. 2021, pp. 1929–1935, pubmed.ncbi.nlm.nih.gov/34378342/#:~:text=Abstract.%20Biotin%20interference%20in%20streptavidin/biotin%2Dbased%20immunoassays%20has, https://doi.org/10.1002/dta.3141. Accessed 16 May 2024.
- Racek, Jaroslav, et al. “False Positive Result of Human Chorionic Gonadotropin Caused by Human Anti-Mouse Antibodies.” Biochemia Medica, vol. 33, no. 1, 15 Feb. 2023, pp. 82–86, www.ncbi.nlm.nih.gov/pmc/articles/PMC9927729/#:~:text=Most%20false%20positive%20hCG%20results, https://doi.org/10.11613/bm.2023.010802. Accessed 3 Apr. 2024.
- Tipped (Tilted) Uterus.” Mayo Clinic, 2020, www.mayoclinic.org/diseases-conditions/female-infertility/multimedia/tipped-uterus/img-20008147. Accessed 21 Aug. 2024.

Struggling with the 8-month sleep regression? Learn why it happens, common signs, and expert tips to help your baby sleep better.

Discover the difference between Braxton Hicks vs contractions. Learn how to identify practice contractions and the best ways to manage them.
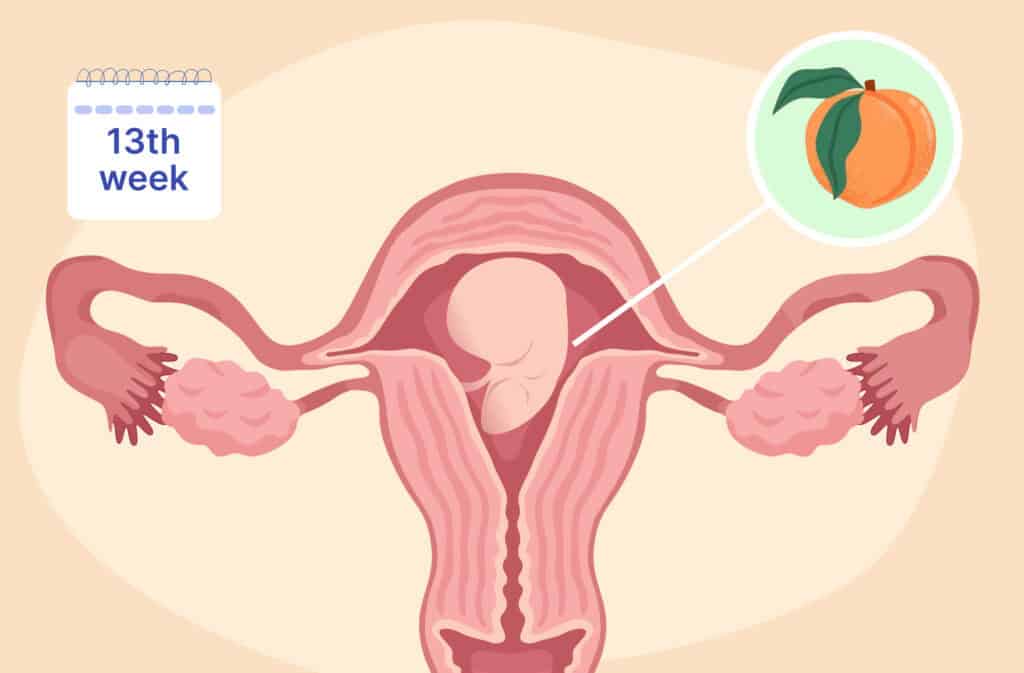
Discover what happens at 13 weeks pregnant, from baby’s development and bump changes to ultrasound insights and common symptoms.

