Femia > Health Library > Pregnancy > Pregnancy health > Vanishing twin syndrome: Causes, symptoms, and impact on the surviving twin
Vanishing twin syndrome: Causes, symptoms, and impact on the surviving twin

- Updated Feb 10, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
- Vanishing twin syndrome (VTS) is a condition that occurs early in pregnancy when one of the twins detected on an ultrasound stops developing, often before 12 weeks. T In most cases, the mother and the surviving twin absorb the tissue from the vanished twin without causing harm. However, in some instances, VTS can lead to complications, depending on the stage of pregnancy when it occurs or if there are underlying issues such as problems with the placenta.
- Symptoms can include light bleeding or cramping, but many women experience no signs at all.
- The surviving twin typically continues to develop normally, and medical monitoring ensures the pregnancy progresses safely.
Vanishing twin syndrome (VTS) was first recognized in 1945. This syndrome causes a pregnancy involving twins to become a pregnancy involving only one embryo. Simply put, it’s when, usually in the first trimester, one of the embryos detected on initial ultrasounds stops developing.
Vanishing twin syndrome is often diagnosed through ultrasound, and it cannot be prevented or treated. As a type of miscarriage, this syndrome can cause stress and grief, even when the second embryo is developing healthily. Maintaining a healthy lifestyle and managing chronic conditions before pregnancy can help reduce the risk of complications, including the loss of an embryo. It’s important to seek both clinical and emotional support throughout the pregnancy to navigate this challenging experience.
Personalized meal plans, symptom tracking, and more with the Femia
What is vanishing twin syndrome?
Vanishing twin syndrome (VTS) is a condition that can occur in the early stages of pregnancy, where one of the embryos or fetuses, initially detected on ultrasound, later becomes undetectable. This occurs when one or more embryos (in the case of triplets or higher-order multiples) stop developing. The tissue of the vanishing embryo is absorbed by the surviving embryo(s), a process that generally does not harm the mother.
VTS is often identified through ultrasound, a technology that has increased the detection rate of this condition. However, it can remain undetected unless an early ultrasound reveals a second embryo that later disappears. The risk of developing VTS is higher in pregnancies resulting from assisted reproductive technologies (IVF), as these often involve the transfer of multiple embryos.
The absorption of the embryo tends to occur more frequently when there are developmental issues or genetic abnormalities in the vanishing embryo. In some cases, VTS can lead to complications in the second trimester, such as growth restriction of the surviving fetus or issues with the amniotic membranes. Therefore, these later losses require more careful monitoring to ensure the health and development of the remaining pregnancy.
👉Find out more: Twin pregnancy belly week by week: What to expect
How does vanishing twin syndrome happen?
Vanishing twin syndrome often happens within the first 12 weeks of pregnancy. The mother may not even be aware that she was carrying twins.
The risk is highest in the first trimester and significantly drops once a fetal heartbeat is established. This phenomenon typically occurs due to developmental abnormalities in one of the embryos, which become noticeable during the first trimester through ultrasound. These abnormalities often lead to the cessation of development of the affected embryo.
A 2003 study reports that the risk for twin miscarriage once the babies’ heartbeats are detected is only around 7%. This risk continues to decrease as the pregnancy progresses.
Experts aren’t 100% sure of the specific causes of the vanishing twin syndrome, although two key explanations have been put forward. These include:
- Major genetic or chromosomal abnormalities, which mean the embryo is not viable.
- Improper cord implantation, although this is rarely the sole cause of the vanishing twin. It is more often associated with overall implantation issues that can affect the development of one embryo.
Additionally, placental development abnormalities or poor attachment of the gestational sac to the uterine lining (endometrium) are also possible contributing factors to VTS. These factors can hinder the proper growth and nourishment of the embryo, leading to its disappearance.
Symptoms of vanishing twin syndrome
The reason for some women not knowing that they had carried twins is that signs of vanishing twin syndrome are pretty similar to symptoms common during the first pregnancy trimester.
Symptoms may include:
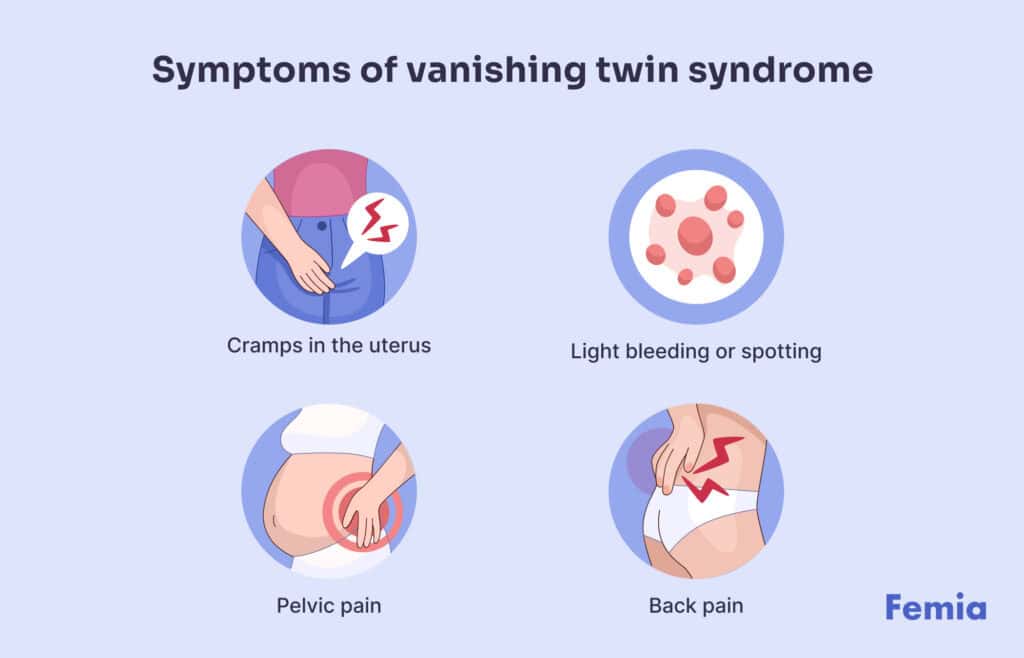
- Cramps in the uterus
- Light bleeding or spotting
- Pelvic pain
- Back pain
Symptoms differ from one woman to another, so you may miscarry one twin with heavy bleeding, light spotting or no symptoms at all.
It’s best to contact a healthcare provider if any of these symptoms appear during pregnancy, especially unexplained bleeding.
How long do you bleed with vanishing twin syndrome?
The duration and the flow of the bleeding with vanishing twin syndrome will vary based on how and when the miscarriage occurs.
In most cases, bleeding may last from a few days to a couple of weeks, but it will depend on the body’s natural process of absorbing or passing the tissue of the absorbed twin.
Some women experience light bleeding that resembles spotting, while for others, it may be heavier and accompanied by cramping.
If the twin disappears very early in pregnancy, the body may reabsorb the tissue with minimal bleeding. However, if the vanishing twin syndrome happens later, the bleeding is likely to be heavier and longer.
To ensure there are no complications and to monitor the health of the surviving twin, make sure you consult a healthcare provider as soon as you notice any changes or experience symptoms.
Diagnosis and ultrasound findings
Vanishing twin syndrome is usually diagnosed during routine ultrasounds in early pregnancy. That is because early ultrasounds may reveal the presence of two gestational sacs, where one appears to be empty or shows signs of a lost twin because of the absence of a heartbeat. These findings typically lead to the diagnosis of vanishing twin syndrome.
As the pregnancy progresses, subsequent ultrasounds usually show only the surviving twin. In some cases, the remains of the vanished twin may not be visible at all, as the body absorbs the tissue completely.
Accurate diagnosis through ultrasound and medical monitoring ensures that the health of the surviving twin is tracked appropriately.
Vanishing twin effect on surviving twin
In most cases, the surviving twin in vanishing twin syndrome develops normally without complications. The body adapts to the loss of one twin, allowing the other fetus to grow and develop.
However, proper medical monitoring is required to ensure the health and normal growth of the surviving twin throughout the pregnancy after absorbing the tissue of the lost one. Studies published by NCBI indicate that vanishing twin syndrome rarely affects the surviving twin’s development or long-term health. However, some studies suggest a possible link between the loss of one fetus and an increased risk of complications in the mother, such as preeclampsia, gestational diabetes, or other health issues. In cases of monozygotic pregnancies (identical twins), there may be a higher risk for the surviving twin due to shared blood circulation.
Emotional and physical effects of vanishing twin syndrome
Vanishing twin syndrome is a type of miscarriage, and it may cause stress and grief when a future mother knows that she carried twins.
If you experience vanishing twin syndrome, you want to give yourself the care needed to mentally and emotionally process the VTS diagnosis. Taking care of yourself, seeking support from family and friends, and receiving medical help when required are essential.
Experiencing grief after knowing about the syndrome might be challenging for some because even though you experienced a miscarriage, you’re still pregnant. But it’s okay to experience mixed feelings, just make sure you process everything you’re feeling.
You may also want to ask your healthcare provider about what to expect as your pregnancy progresses after vanishing twin syndrome. Knowing symptoms and having clarity about what to expect over the next months can help you reduce your stress and focus on your health and emotional well-being.
👉Find out more: Best positions to relieve gas while pregnant for immediate comfort
Medical management and follow-up care
Although no specific treatment is usually required for vanishing twin syndrome, the approach may vary depending on the timing of the twin’s disappearance and any additional complications. In many cases, the pregnancy will be monitored more closely after the absorption of the second twin to ensure the health and well-being of the surviving one. For example, in the second trimester, additional tests and assessments of placental function may be necessary to monitor for potential complications, such as growth restriction or placental issues. This usually involves:
- Conducting additional ultrasounds and checkups to track the development and growth of the remaining fetus, as well as assess placental function and the amount of amniotic fluid. These ultrasounds are crucial to ensure that the surviving fetus is developing properly and to monitor for any signs of intrauterine growth restriction.
- Providing mental health services, as it’s important to process the stress and grief that may occur as a result of Vanishing Twin Syndrome (VTS). Support from healthcare professionals can help manage emotional well-being during this challenging experience.
Frequent monitoring allows healthcare teams to detect and address potential complications early, ensuring the pregnancy progresses as safely as possible. In most cases, pregnancies with a surviving twin continue without significant issues, but individualized care helps reassure and support the expecting parent throughout the process.
Personalized meal plans, symptom tracking, and more with the Femia
Questions from the Femia community
Can vanishing twin syndrome occur in the second trimester?
It is rare but possible for a twin to vanish after the first trimester. However, it most often happens during the first trimester. It's important to note that pregnancies involving vanishing twin syndrome after the first trimester are considered high-risk. If the loss of the second twin happens in the second trimester, the healthcare team needs to closely monitor the health of the surviving twin to watch for any signs of complications.
Can you miscarry one twin without symptoms?
Yes, although bleeding and spotting are common symptoms, it is possible to have Vanishing Twin Syndrome with no symptoms, especially when the twin disappears in the very early stages of the pregnancy. The syndrome often progresses without noticeable signs, particularly in the first trimester. However, in the second trimester, symptoms such as bleeding or a decrease in fetal movement may occur and should be closely monitored.
Does vanishing twin syndrome affect the later stages of pregnancy?
No, in most cases, if no complications arise during pregnancy, the condition does not affect the later stages. With proper medical monitoring and care, the risks to the surviving fetus are minimal, and the pregnancy is likely to progress normally. Regular follow-ups ensure that any potential issues, such as growth restriction or placental problems, are addressed early.
Will I have a higher chance of vanishing twin syndrome in a future pregnancy?
The short answer is no. Current evidence does not suggest that having vanishing twin syndrome increases the risk of having it in future pregnancies. Each pregnancy is unique, and the occurrence of VTS is generally considered a one-time event.
Can vanishing twin syndrome cause a false negative pregnancy test?
False negative pregnancy tests are uncommon and usually occur due to early testing or improper usage of the test. There is no strong evidence directly linking Vanishing Twin Syndrome to false negatives. While being pregnant with twins might rarely lead to a false negative result, the most common reasons for inaccurate test results are testing too early or not following the test instructions properly.
The bottom line
Vanishing twin syndrome is a type of miscarriage that, while it can cause grief for the mother, rarely affects her health or that of the surviving twin. The condition often occurs early in pregnancy. The vanished twin’s tissue is harmlessly absorbed. Regular medical monitoring ensures the health of the remaining twin, while emotional support is essential to help a future mother navigate feelings of grief or loss. Despite the initial challenges, most pregnancies after vanishing twin syndrome result in healthy outcomes for the surviving twin.
References
- “Vanishing Twin Syndrome: Causes, Symptoms & Diagnosis.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/23023-vanishing-twin-syndrome.
- “Vanishing Twin Syndrome.” American Pregnancy Association, 26 Apr. 2017, americanpregnancy.org/healthy-pregnancy/multiples/vanishing-twin-syndrome/.
- Tummers, P. “Risk of Spontaneous Abortion in Singleton and Twin Pregnancies after IVF/ICSI.” Human Reproduction, vol. 18, no. 8, 1 Aug. 2003, pp. 1720–1723, https://doi.org/10.1093/humrep/deg308.
- Cleveland Clinic. “Ovulation, Conception & Getting Pregnant | Cleveland Clinic.” Cleveland Clinic, 2019, my.clevelandclinic.org/health/articles/11585-pregnancy-ovulation-conception–getting-pregnant.
- “Vanishing Twin Syndrome.” American Pregnancy Association, 26 Apr. 2017, americanpregnancy.org/healthy-pregnancy/multiples/vanishing-twin-syndrome/.
- Zamani, Zarlakhta, and Utsav Parekh. “Vanishing Twin Syndrome.” PubMed, StatPearls Publishing, 2021, www.ncbi.nlm.nih.gov/books/NBK563220/.
How many eggs do women have and how does their amount change with age? Here is a guide to help you get a better understanding of your fertility.

Understanding the 4 stages of labor can help you know what to expect when you give birth.

Learn to detect ovulation pain as a sign of your fertile window to increase your chances of pregnancy success.

