Femia > Health Library > Pregnancy > Pregnancy week by week > Your pregnancy checklist: Week-by-week guide to preparing for baby
Your pregnancy checklist: Week-by-week guide to preparing for baby

- Updated Feb 11, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
Start with confirming the pregnancy and discussing prenatal vitamins early on, incorporate a balanced diet and regular exercise by the 8th week, and plan nursery details and prenatal classes by the 13th week.
With so many changes and milestones happening along the pregnancy journey, it’s totally okay to feel both excited and overwhelmed. Medical visits, pregnancy classes, and worries about a baby—every new thing can cause more and more stress, but you are not alone.
Having a pregnancy checklist can help you keep track of everything and ease your worries, ensuring a stress-free and smooth pregnancy experience.
In this guide, we’ve broken down the pregnancy checklist by week, providing a detailed guide on each stage, so you don’t have to worry about even the smallest thing being missed. Let’s get into it.
First trimester (weeks 1–13)
Weeks 1–4: initial preparations
At the very beginning, it’s essential to confirm that you are indeed expecting. For that, you may want to:
- Find a prenatal care provider in your insurance network.
- Write down the date of your last period.
- Check your health insurance policy to explore what prenatal and childbirth care is covered.
- Schedule an appointment with a healthcare provider to discuss the next steps.
For example, a doctor may ask for a health checkup, including blood work, to confirm pregnancy and identify any early deficiencies in key vitamins. According to the American College of Obstetricians and Gynecologists (ACOG), women should begin taking folic acid at least a month before conception, not just after confirming pregnancy. This early start helps ensure the best possible health outcomes for both the mother and the developing baby.
With Femia, you will get personalized insights every step of the way
Weeks 5–8: health and wellness
As you progress into the second month, maintaining a healthy lifestyle becomes a must-have. Here is what you need to know for the pregnancy planner checklist at 5–8 weeks:
- Focus on eating a balanced diet that is rich in essential nutrients. Consider adding food containing iron (tofu, soybeans, spinach), calcium (milk, cheese and other dairy foods), and DHA (chia seeds, salmon, flax seeds, walnut).
- Avoid harmful substances like alcohol and tobacco, since they negatively impact your baby’s development.
- Start adding regular, gentle physical activity, such as prenatal yoga or walking, to your routine. This is beneficial for a healthy pregnancy and can also help you manage some pregnancy symptoms.
- This is also a good time to start researching hospitals and healthcare providers to find the place where you will deliver your baby. You can consider different birthing options aside from those offered at the hospital—for example, birthing centers or home births. Choose one that aligns with your preferences for prenatal care.
👉Find out more: Why choline is essential during pregnancy: Benefits, sources, and supplements
Important note: ACOG advises choosing locations with certified midwives or obstetricians, rather than opting for home births unless there are clear medical indications. Home births can be associated with increased risks for both the mother and baby in the event of unforeseen complications.

@femia.fertility 5 key steps for a successful pregnancy journey: 🥗 Balance your diet 👟 Walk 8K steps daily 💧 Stay hydrated 🧘♀️ Meditate to relieve stress 🤸♀️ Do pelvic exercises Your dream of parenthood starts with taking care of YOU. Follow Femia for more on fertility-friendly nutrition, exercises, and meditation tips. #ttccommunity #pregnancyjourney #ttcjourney #fertilityjourney #fertilityapp #ultrasound #dreambaby #momtobe ♬ Beautiful Is You - Karissa Ella
Weeks 9–13: early planning
Once you establish your healthy lifestyle and choose some options for delivery, you may want to move further and think about the future in more detail. Here are some things that you may start doing during these weeks:
- Familiarize yourself with the prenatal tests that doctors may recommend during this period. The following screenings and tests are performed at 9–14 weeks to determine if the fetus may have a birth defect like Down syndrome:
| The first-trimester serum screening | Helps identify a pregnancy with an increased risk of Down syndrome. Involves a blood test and an ultrasound. |
| Cell free fetal DNA screening |
Identifies if the fetus has abnormalities in sex chromosomes and involves a blood test. |
| Nuchal translucency ultrasound test |
Optional ultrasound that measures the amount of fluid at the back of the fetus’ neck to calculate if the baby has a chromosomal or genetic variant. |
| Maternal serum (blood) tests | Measures pregnancy-associated plasma protein and human chorionic gonadotropin. |
- Join a prenatal exercise class, such as yoga or pilates.
- Plan a nursery, think about themes and the overall layout, and use Pinterest to get some ideas.
- Begin brainstorming baby names and compiling a list of your favorites.
Second trimester (Weeks 14–27)
Weeks 14–18: mid-pregnancy preparations
It is common for future mothers to feel more energized and relieved when entering the second trimester because of the reduced risk of miscarriage. So, here are some things it is best to plan at this stage:
- Discuss with your healthcare provider the prenatal tests and screenings that might be offered during these weeks. The key ones include:
| Maternal serum AFP | A blood test to measure AFP, a protein produced by the fetal liver found in the fluid surrounding the fetus. |
| Neural tube defects test | Also known as amniocentesis. Performed to identify if the fetus has a neural tube defect. |
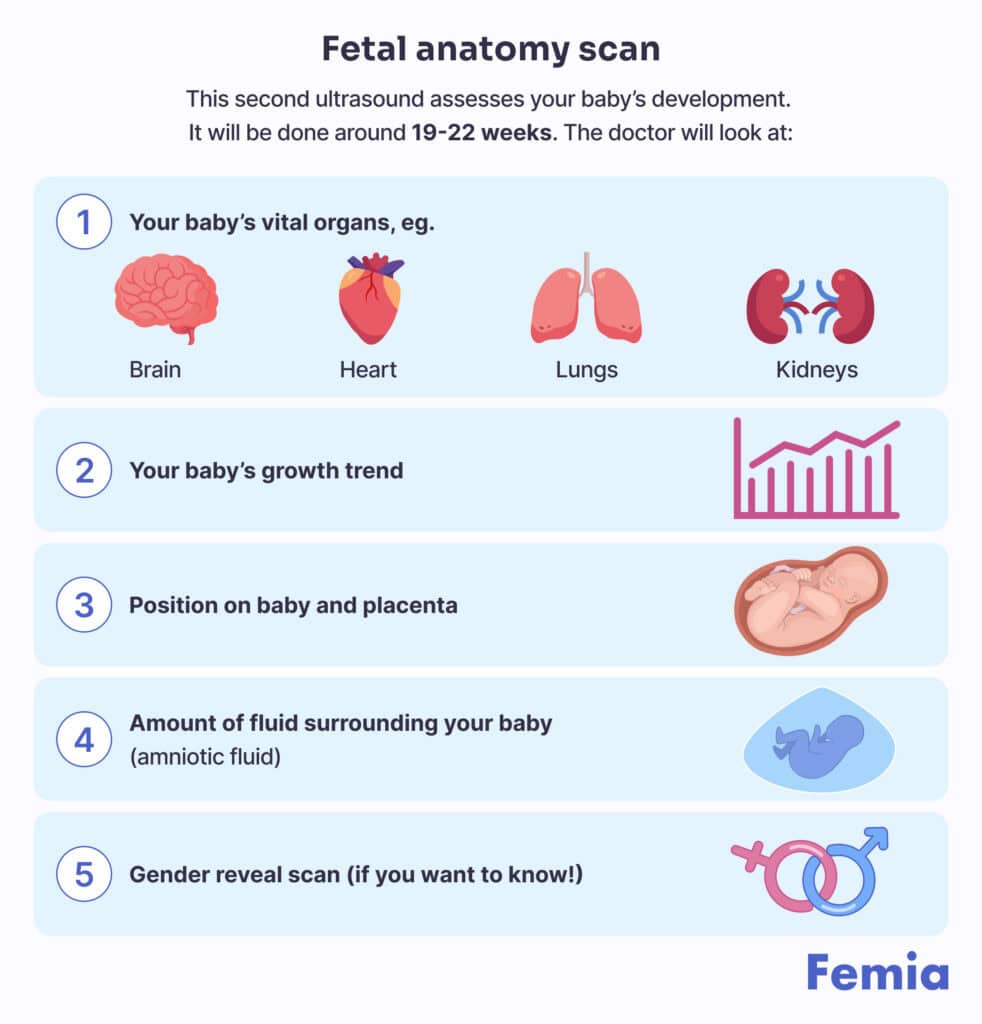
| A 18- to 20-week anatomy scan | Measures fetal growth and activity and checks the amount of amniotic fluid. |
- Familiarize yourself with the vaccines that can be done during the second trimester, and discuss them with your doctor. For example, these can be vaccinations against influenza and COVID-19.
- Plan a maternity or paternity leave. Discuss it with your partner and then with HR, so you can inform your workplace about leave dates and understand your rights and benefits.
- Plan your second prenatal visit, and discuss any new symptoms or concerns with your healthcare provider.
- This is also a good time to start building your maternity wardrobe. Select comfortable clothes that will support your growing belly.
Weeks 19–22: preparing the home
As you approach the halfway mark, you may want to focus on preparing a home for a baby’s arrival:
- Look into childcare options, such as a nanny or daycare. You may want to sign up for a daycare early, especially if you want a specific and popular kindergarten.
- Start setting up the nursery.
- Choose essential furniture pieces like a crib, changing table, and storage for baby items.
- Baby-proof your house: install smoke and carbon monoxide detectors, cover electrical outlets, install safety gates, secure furniture, prevent slipping, remove choking hazards, and store batteries away.
- Register for or buy baby items, including strollers, car seats, diapers, and baby monitors.
- You may also want to create a list of items you buy and those you would like to get from family and friends if you have this opportunity.
Weeks 23–27: education and support
In these weeks, prioritize education and building a support network. Some tests still need to be done these weeks as well.
- A glucose challenge screening test is done to check for gestational diabetes that can develop during pregnancy.
- Attend prenatal classes that educate on childbirth, breastfeeding, and newborn care.
- Consider joining support groups, both local and online, so you can get emotional support and don’t feel like you deal with everything alone. These groups may also provide helpful advice.
- It’s the best time to discuss your birth plan preferences with a chosen healthcare provider. Discuss pain relief options, labor positions, and any specific preferences you have for the birth process.
- Start looking for a pediatrician.
Third trimester (Weeks 28–40)
Weeks 28–32: final preparations
Entering the third trimester means you are ready to finalize your preparations for the baby’s arrival:
- Start fetal kick counts: it’s best to download an app so you can count the baby’s movements every day, preferably around the same time. But, you can also do it on paper!
- Finish the nursery setup, and ensure you have all essential items, from furniture to clothing and toiletries.
- Consider postpartum support or childcare if required, so you always have a plan B when the baby arrives.
- Create a birth plan, and discuss it with your partner. Explain how you see your birth, discuss whether you want your partner to be with you during delivery, and what pain-relief options you’re considering.
- You may also want to prepare and freeze meals, so you won’t worry about getting enough nutritional food during the busy postpartum period.
Weeks 33–36: health and logistics
At this stage, you will want to focus on the logistics of childbirth. Here are some things to cross off of your pregnancy to-do list:
- Pack a hospital bag. Include comfortable clothing, toiletries, documents, and items for the baby.
- Pre-register at the hospital or birthing center, so you don’t have to waste time when the time comes.
- Confirm your birthing plan with a healthcare provider, revisiting any last-minute details and ensuring everyone is on the same page.
- Download a contraction timer, and discuss signs of labor with a doctor, so you know what to do and when.
Weeks 37–40: ready for baby
These will be your last weeks, and everything should be ready and planned for the baby’s arrival. However, here are some last-minute things for your to-do list before baby arrives:
- Explore what screening tests your hospital routinely gives newborns. Some of the key tests are blood, heart, and hearing screening.
- Talk to a healthcare provider about any additional tests you would like run.
- Do your vaginal Group B strep test (this can be done from 35 to 37 weeks).
- Get your whooping cough (Tdap) vaccine (this can be done from 27 to 36 weeks).
- Screen for signs of depression during pregnancy, and consult a psychologist to get more information if you have any signs and worries. Although symptoms may be caused by changing hormones, consider checking yourself for fatigue, sleep problems, excessive anxiety, irritability, getting angry easily, or feeling tearful.
- Install car seats in your vehicle, and check that they are securely fastened.
- Make any last-minute preparations for your home.
- Check yourself for signs of labor, like regular contractions and water breaking.
- Draft a plan for when labor starts, discussing who to call, how to get to the hospital, and where your hospital bag will be.
Postpartum checklist
First week: immediate needs
- In the first week after delivery, you should focus on your recovery and bonding with your newborn.
- Sleep while the baby sleeps, or ask your partner to help manage the sleep schedule, so you can get as much sleep as you can during the very first few weeks.
- Consider scheduling the baby’s first pediatrician visit to ensure they are healthy and thriving.
- Monitor your health and well-being as well, checking for signs of postpartum depression or complications.
Please reach out to a healthcare provider if you have any concerns about yourself or your baby.
First month: adjustments
At this time, there will be some ups and downs while you try to adjust to a new routine. So, here are some tips to help you make the process less stressful:
- Work on establishing a feeding routine. Whether you have chosen breastfeeding or formula, having some kind of schedule will greatly help you in getting some rest as a new mother.
- Seek lactation support if you encounter any issues with breastfeeding—this could be from a healthcare provider, the forums we discussed above, or a specialist in this field.
- Take care of your mental health by checking for symptoms of postpartum depression, and seek help when needed.
- Joining new parent groups or talking to other parents may also be helpful in providing comfort and advice.
- Do not forget to thank and appreciate yourself for navigating this new and challenging phase.
👉Find out more: Understanding lactation: Signs your milk is coming in during pregnancy
With Femia, you will get personalized insights every step of the way
Questions from the Femia community
When should I start preparing for my baby's arrival?
It depends on when you confirm that you are pregnant. However, the general recommendation is to start preparing as soon as you find out you are pregnant. Early planning helps reduce stress and allows you to smoothly spread tasks out over the course of your pregnancy.
How can I ensure that I don't forget any important tasks?
It's best to create and follow your preparing-for-baby checklist once you know you are carrying. You can also monitor and review your checklist each month to help you stay on track. Using a planner or a pregnancy app is also useful in organizing everything for your baby's delivery.
Are there specific items I need to baby-proof my home?
Yes; baby-proofing is essential. These often include safety gates, outlet covers, cabinet locks, and securing heavy furniture to prevent tipping. Include all these items on your checklist, and indicate when to install them.
What should I do if I feel overwhelmed by the pregnancy preparations?
If you feel stressed and overwhelmed, don't hesitate to seek help. Ask your family and friends for support, and join groups. You can also talk with your healthcare provider to get support and information.
The bottom line
Using a detailed pregnancy checklist allows parents-to-be to navigate the pregnancy journey with confidence and ease, ensuring they are well-prepared for each stage. By following a structured plan, expectant parents can focus on enjoying the experience and preparing for their new addition without unnecessary worry.
References
- Marshall, Nicole E., et al. “The Importance of Nutrition in Pregnancy and Lactation: Lifelong Consequences.” American Journal of Obstetrics and Gynecology, vol. 226, no. 5, 2021, pp. 607–632, pubmed.ncbi.nlm.nih.gov/34968458/, https://doi.org/10.1016/j.ajog.2021.12.035.
- Odendaal, H J, et al. “Dangers of Smoking Cigarettes and Drinking Alcohol during Pregnancy.” South African Medical Journal, vol. 110, no. 11, 28 Oct. 2020, p. 1066, https://doi.org/10.7196/samj.2020.v110i11.14738.
- Guinhouya, Benjamin C., et al. “Beneficial Effects of Maternal Physical Activity during Pregnancy on Fetal, Newborn, and Child Health: Guidelines for Interventions during the Perinatal Period from the French National College of Midwives.” Journal of Midwifery & Women’s Health, vol. 67 Suppl 1, no. Suppl 1, 1 Nov. 2022, pp. S149–S157, pubmed.ncbi.nlm.nih.gov/36480665/, https://doi.org/10.1111/jmwh.13424.
- Mayo Clinic Staff. “Prenatal Testing: Is It Right for You?” Mayo Clinic, 25 Aug. 2020, www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-testing/art-20045177.
- Mayo Clinic. “Miscarriage – Symptoms and Causes.” Mayo Clinic, 2021, www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptoms-causes/syc-20354298.
- Jabaz, Doaa, and Mohammed Abed. “Sonography 2nd Trimester Assessment, Protocols, and Interpretation.” PubMed, StatPearls Publishing, 2021, www.ncbi.nlm.nih.gov/books/NBK570574/.
- Mayo Clinic. “Labor and Delivery: Pain Medications.” Mayo Clinic, 2017, www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/labor-and-delivery/art-20049326.
- “Signs of Labor: Know What to Expect.” Mayo Clinic, www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/signs-of-labor/art-20046184.
- Mayo Clinic. “Postpartum Depression – Symptoms and Causes.” Mayo Clinic, 24 Nov. 2022, www.mayoclinic.org/diseases-conditions/postpartum-depression/symptoms-causes/syc-20376617.

What are the key postpartum needs for mom? Click to find an all-rounded checklist of the essential things you might need for recovery, hygiene, and well-being.
Discover the symptoms, causes, treatment and misconceptions of low testosterone in women, including age-related testosterone levels and when to consult a doctor.
Let’s learn how long does it take for sperm to reach an egg, when implantation happens and factors affecting the speed.

