Femia > Health Library > Your cycle > Health > Endometriosis self-care: tips for managing symptoms and boosting fertility
Endometriosis self-care: tips for managing symptoms and boosting fertility

- Updated Feb 10, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
- Heat therapy: Use heating pads or warm baths to ease pelvic pain and cramping.
- Regular exercise: Gentle activities like yoga or walking can reduce inflammation and improve well-being.
- Anti-inflammatory diet: Focus on foods rich in omega-3s (like fish and nuts) and avoid processed, high-sugar foods.
- Stress management: Practice relaxation techniques like meditation, deep breathing, or mindfulness to manage stress.
- Pain relievers: Over-the-counter medications, such as ibuprofen, can help alleviate discomfort.
- Track symptoms: Keep a journal of your pain, mood, and cycle patterns to share with your doctor.
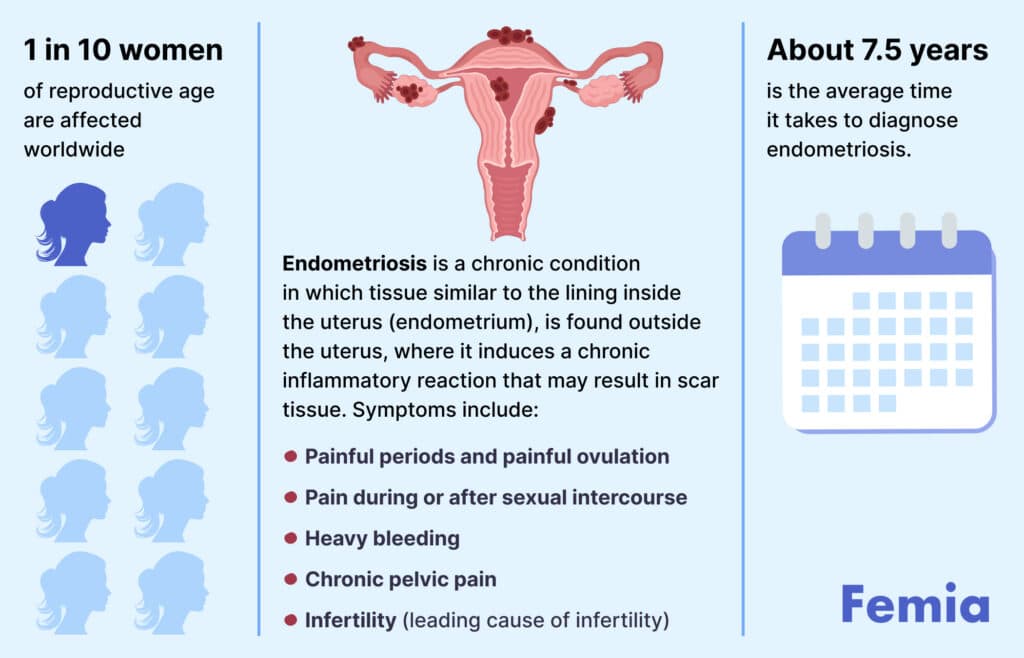
Endometriosis is a chronic condition under which uterine tissue expands outside the uterus, often affecting other organs, including the ovaries, fallopian tubes, and tissue lining the pelvis. Less frequently, it can also grow beyond pelvic organs.
The latest data from the World Health Organization reveal that endometriosis affects around 10% (190 million) of girls and women globally. Symptoms can vary in terms of their severity and the level of impact they have on a woman’s life. Nevertheless, current treatments and quality self-care, based on healthcare provider recommendations, can make living with endometriosis easier.
In this guide, we’ll share effective endometriosis self-care tips that can complement your doctor’s recommendations to help you manage symptoms and improve your quality of life.
Femia helps you understand your symptoms and when to take action
Endometriosis symptoms
Common symptoms include:
- Lower belly, pelvic, or back pain;
- Pain during or after sex;
- More severe period pain that might interfere with everyday life;
- Heavy bleeding;
- Pain when urinating during menstruation;
- Overall decline in health, including diarrhea, constipation, sickness, etc.
Endometriosis might also compromise fertility in some females, as it might damage the reproductive tract and reduce the ovarian reserve.
👉Find out more: How to get pregnant with endometriosis naturally
Endometriosis self-care advices
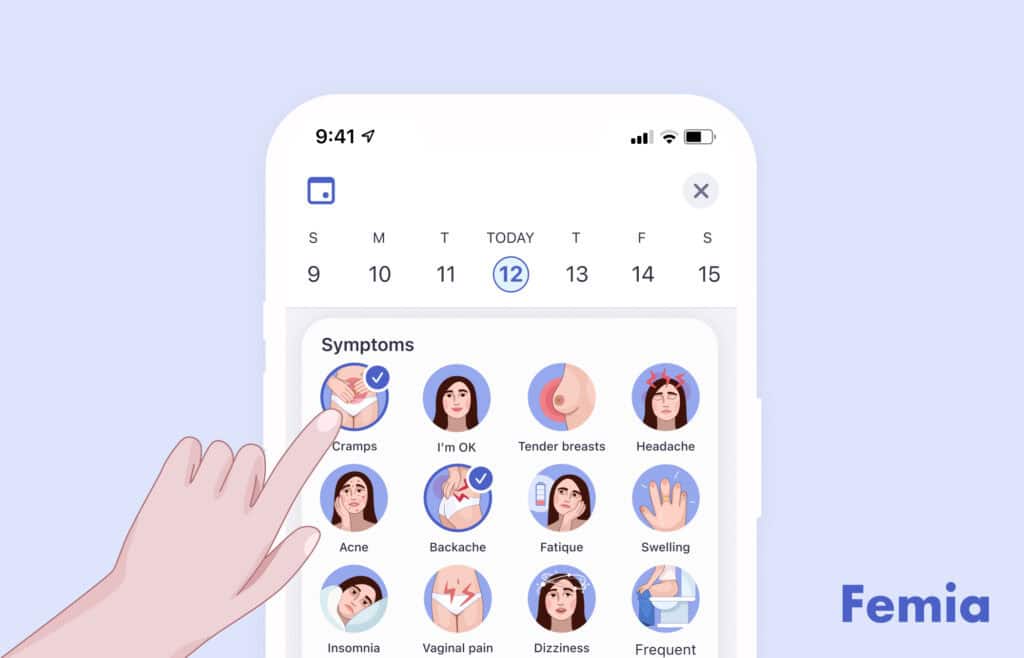
1. Symptoms tracking
Regular symptom monitoring and assessment is an important element of endometriosis self-care. For women who record and analyze their symptoms (and their severity), it can offer a validation of the physiological nature of their symptoms and their link to different phases of a menstrual cycle. This can help locate any patterns or cyclical symptom severity, so you can be better prepared for how this condition might affect your quality of life during certain times and ensure optimal care.
So, the first thing you can consider doing as self-care is to start recording how you feel (both physically and mentally) during different stages of your cycle. This might help you gain a better understanding of your condition.
2. Pain management
For many women, living with endometriosis means having to deal with chronic pain. The following practices might help you manage your pain symptoms:
- Heat therapy. The most common areas to feel endometrial pain are the stomach, lower back, abdomen walls, and pelvic floor. Heat can relax these muscles and reduce cramping. Consider using different methods of heat application to soothe pain, such as taking warm baths, using heating pads, wearing heat wraps, etc.
- Over-the-counter pain relief. When pain symptoms get too intense, it can be a good idea to use some over-the-counter medicines. Most often, women with endometriosis are recommended to use nonsteroidal anti-inflammatory drugs (NSAIDs) as first-line treatment. These medicines are effective for pain management and have few side effects.
- Alternative therapies. When you need to break the pain cycle, it can be beneficial to try alternative approaches, such as acupuncture, chiropractic care, physical therapy, biofeedback, and others.
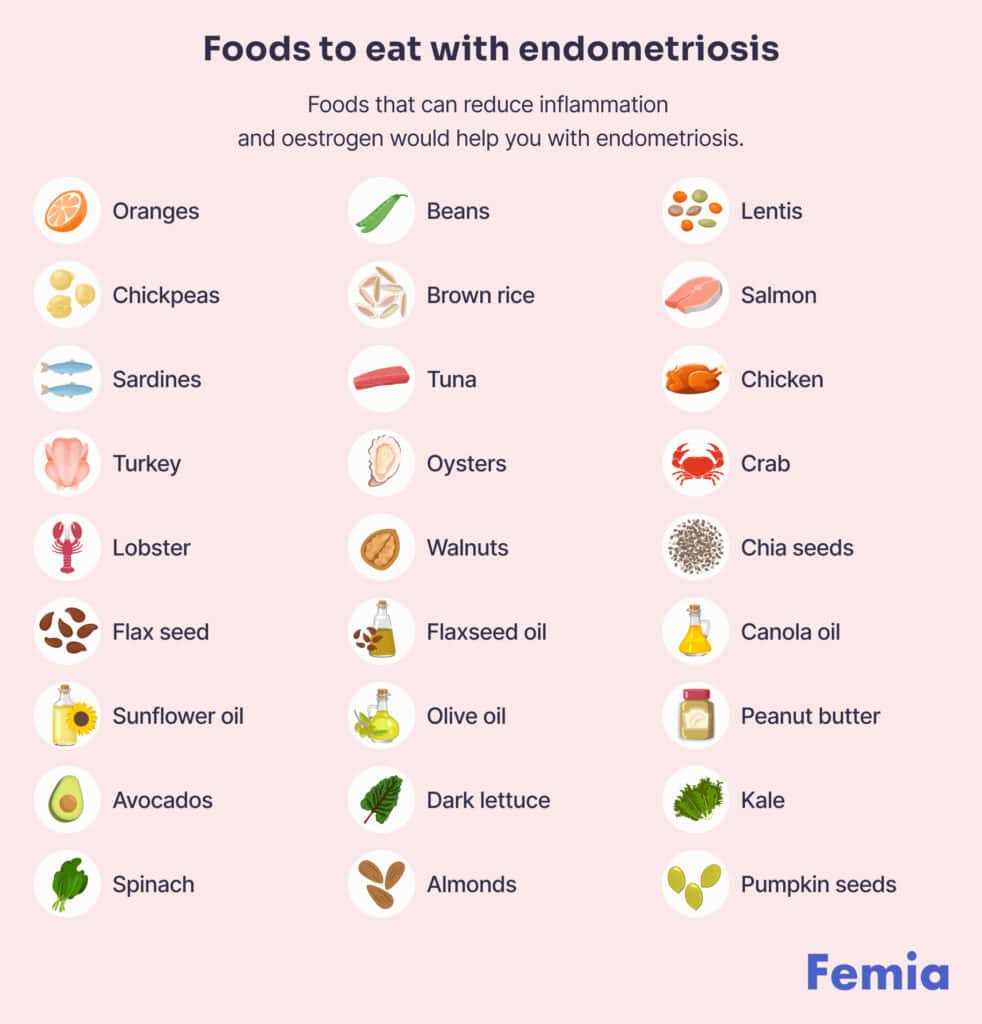
3. Diet changes for endometriosis
Comfortable living with endometriosis may also require some diet adjustments:
Anti-inflammatory diets
Endometriosis often causes inflammation in the pelvic area, which is why dietary plans that reduce inflammation might be a good practice. The key aspects of such diets are:
- Stabilizing insulin with the help of non-starchy vegetables (e.g. carrots, broccoli, cabbage, asparagus, etc.), whole grain foods (e.g. brown rice, whole wheat pasta, etc.), and high protein foods (e.g. skinless poultry, nuts, seeds, beans, etc.).
- Reducing intake of omega-6 fatty acids (e.g. oils, mayonnaise, etc.).
- Balancing omega-6 macronutrients with higher omega-3 intake (e.g. spinach, salmon, soybean, etc.).
Foods that help relieve pain
A dietitian from the University of Vermont Medical Center recommends that people with chronic pain include the following foods into their diets:
- dark, deep-colored vegetables and fruits (e.g. strawberries, beets, broccoli, etc.),
- high-fiber plant proteins like nuts and seeds, hearty whole grains, and omega-3 fatty acids.
4. Endometriosis supplements
For the sake of complementary treatment and overall health improvement, females with endometriosis may also want to enrich their diets with the following vitamins and supplements:
- Magnesium
- Propolis
- Zinc
- Vitamin D
- Vitamin C
- Vitamin E
- Omega 3
- Curcumin
- Probiotics
- Quercetin
- N-acetylcysteine
- Alpha lipoic acid
- Resveratrol
- Selenium
- Epigallocatechin-3-gallate
5. Find your best exercise
Regular, gentle exercise is often linked to pain-relieving features and overall wellbeing improvement. So, if you are looking for more endometriosis tips, consider engaging in low-impact physical activities.
Namely, studies revealed the positive effects of hatha yoga on daily pain and quality of life among women with endometriosis. Stretching and similar relaxation activities have also been shown to reduce pain symptoms while promoting additional mental benefits.
Other activities that might be helpful include pilates, water aerobics, swimming, walking, and similar low-impact exercises.
6. Stress management
Endometriosis is widely associated with increased stress levels, which is why stress management is also a crucial part of self-care. To reduce stress and support mental wellness, you can consider trying various stress management techniques:
- Meditation. Studies reveal that regular meditation practice helps promote mindfulness, mental wellbeing, and decreased perceived stress. It is also linked to anxiety reduction.
- Breathing techniques. Deep breathing is shown to be an effective way to improve mood and reduce stress, based on self-reported participant evaluations. It also shows a positive impact on objective parameters, such as cortisol levels and heart rate.
- Mindfulness. Regular mindfulness practices are frequently used for treating depression and anxiety, as well as improving overall wellbeing.
- Magnesium baths. Magnesium is considered to help control neurotransmitters, cortisol levels, and stress response system. Taking baths with it can help you reduce stress, relax and revive your muscles, and also reduce other symptoms like pain and inflammation.
7. Talk about sex life with your partner
Open communication with your partner about cramps, pain levels, comfort, and preferences is crucial. Discussing what feels good and what doesn’t can help create a supportive environment.
Exploring alternative forms of intimacy, such as cuddling, kissing, or non-penetrative sex, can enhance connection while minimizing discomfort. It’s also helpful to be mindful of your body’s signals; scheduling intimate moments when you’re feeling your best can lead to more satisfying experiences.
Ultimately, prioritizing mutual understanding and respect in your sexual relationship fosters intimacy and strengthens your bond.
Femia helps you understand your symptoms and when to take action
8. Positions to help endometriosis pain
When you experience pain and discomfort caused by endometriosis, certain yoga positions may help bring faster relief.
- Child’s pose. Helps lengthen your spine and release tension in the back muscles, while also opening your hips and relieving tension in the pelvis.
- Cat-cow pose. Stretches the spine, torso, and neck while providing soft stimulus for the abdominal organs. It also helps open the chest to encourage deep, stress-relieving breathing.
- Cobra pose. Opens the shoulder blades and neck, releases the spine, and improves circulation. It also helps relieve stress and lower back pain.
In addition to yoga poses, you can consider practicing pelvic tilts and gentle stretching. These exercises can help strengthen and stretch your pelvic floor, reducing discomfort and pain.

9. How to sleep with endometriosis pain
Pain and discomfort caused by endometriosis may sometimes interfere with healthy sleep. Here are some endometriosis tips that can help you improve sleep quality:
- Find comfortable sleeping positions. A good sleep position can help ensure muscle relaxation, release any tension, and relieve pain. Some of the best positions to try for pain are sleeping on your back or sleeping on your side with a pillow between your knees.
- Create an optimal sleep environment. Your sleeping environment can also improve the quality of sleep. To optimize sleep quality, consider investing in a good mattress that can provide additional support and help avoid awkward positions of your spine and neck. A good pillow can reduce the strain on your neck and head, too. To make your sleep environment more comfortable and calming, you might also consider tweaking room temperature and lighting, decluttering your room, and avoiding the use of electronics during bedtime.
- Establish nighttime routines. Well-established routines are linked to lower stress, improved mental and physical health, and better sleep. To improve your quality of sleep, you can consider establishing fixed nighttime routines that promote relaxation. For example: deep breathing, mindfulness practices, meditation, guided imagery, etc.
10. Find your doctor
Finding a good doctor is essential for effective management of endometriosis, as a knowledgeable healthcare provider can offer tailored treatment options and support. A strong doctor-patient relationship fosters open communication, ensuring that your concerns are heard and addressed, which is vital for your overall well-being.
Questions from a Femia community
Can exercise worsen endometriosis pain?
Physical exercises can be a double-edged sword in addressing endometriosis pain. Regular activity can provide pain relief, while also reducing inflammation and improving circulation. Also, regular exercising is linked to increased endorphin release, which promotes natural pain relief and helps manage stress. Still, certain kinds of physical activity can worsen pain and other symptoms, which is why it’s recommended to opt for gentle, low-impact activities like yoga, stretching, walking, and swimming.
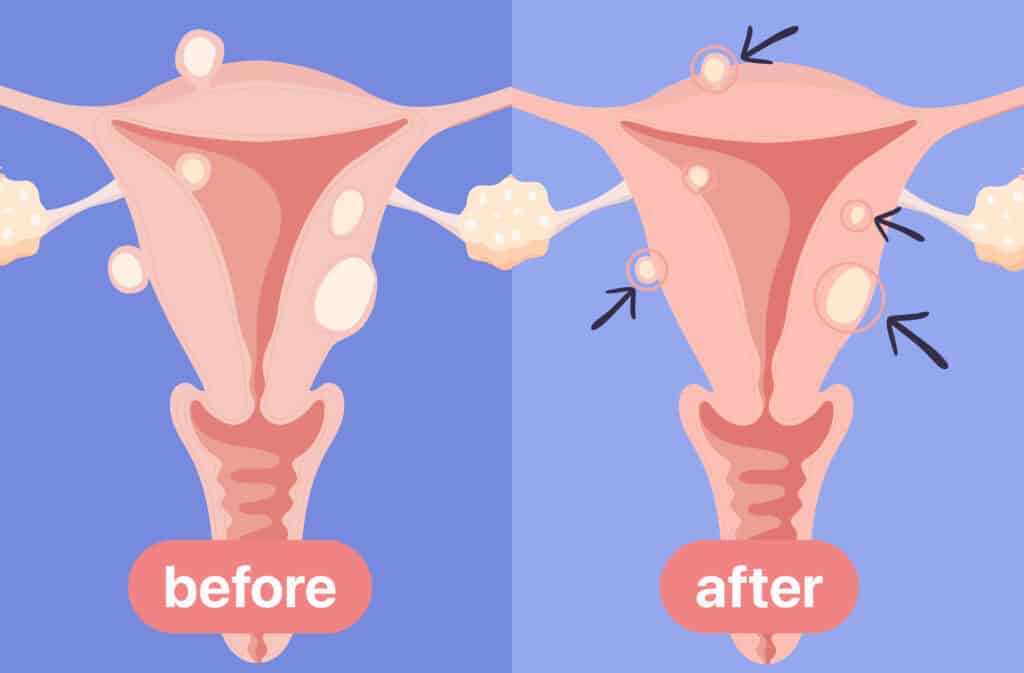
How does endometriosis affect fertility?
Endometriosis causes inflammation in the pelvic area, which can also result in the development of scar tissue, reduced ovarian reserve, and other changes in the female reproductive system. This can affect an egg’s ability to travel through the fallopian tube and get fertilized. So yes, this condition can potentially impact your fertility. To prevent or minimize this impact, it’s suggested to address endometriosis symptoms correctly (through healthcare providers’ recommendations and self-care) and work with fertility specialists.
👉Find out more: How to get pregnant with endometriosis naturally
Can endometriosis go away on its own after menopause?
Endometriosis is typically believed to affect females during their reproductive age (aka, until menopause). Due to decreased estrogen levels, endometrial tissue may not have enough stimuli to grow after menopause, which is why the symptoms of endometriosis often improve at this stage. However, it doesn’t always completely go away.
When should I consider surgery for endometriosis?
You should consider surgery for endometriosis if you experience severe pain that is not relieved by medication, if you have significant symptoms affecting your quality of life, or if you have fertility concerns related to the condition. Surgery may also be recommended if other treatments, such as hormonal therapies, have not been effective in managing your symptoms. Consulting with a specialist can help determine the best course of action for your individual situation.
Is drinking a lot of water good for endometriosis?
Drinking plenty of water can be beneficial for individuals with endometriosis, as proper hydration helps support overall health and may reduce bloating and inflammation. However, it’s important to maintain a balanced diet and consult with a healthcare provider for a comprehensive management plan.
The bottom line
Endometriosis is a common condition that can affect females any time during reproductive age. It is often linked to pain, sickness, and other tangible effects on women’s quality of life. Luckily, improving the quality of life and minimizing endometriosis symptoms is possible thanks to timely and quality healthcare consultation and treatment, plus regular and effective self-care.
The core elements of endometriosis self-care include:
- Symptoms tracking;
- Proper diet and nutrition;
- Low-impact physical activity;
- Stress management.
With this guide at hand, you have a list of strategies and tips for providing yourself with proper care. Consider using the tips from this guide to establish a solid self-care routine to complement your healthcare provider’s recommendations and make living with endometriosis more comfortable. With treatment and the right self-care practices, you can improve your quality of life and enhance your chances of conception, too.
References
- “Endometriosis.” World Health Organization, 24, Mar. 2023. https://www.who.int/news-room/fact-sheets/detail/endometriosis.
- “GYNECOLOGY. Endometriosis.” Children’s Hospital Colorado. https://www.childrenscolorado.org/conditions-and-advice/conditions-and-symptoms/conditions/endometriosis/#:~:text=Endometriosis%20can%20affect%20females%20of,uterus%20and%20surrounding%20pelvic%20tissues.
- Garcia-Fernandez J, García-Velasco JA. “Endometriosis and Reproduction: What We Have Learned.” Yale J Biol Med, 30, Sep. 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7513434/.
- Jones G, Jenkinson C, Kennedy S. “The impact of endometriosis upon quality of life: a qualitative analysis.” J Psychosom Obstet Gynaecol, Jul. 2004. https://pubmed.ncbi.nlm.nih.gov/15715035/.
- Sears B. “Anti-inflammatory Diets.” J Am Coll Nutr, 2015. https://pubmed.ncbi.nlm.nih.gov/26400429/.
- Emily Stone. “6 Food Tips for Pain Relief.” The University of Vermont Health Network, 12, Apr. 2024. https://www.uvmhealth.org/healthsource/6-food-tips-pain-relief.
- Yalçın Bahat P, Ayhan I, Üreyen Özdemir E, İnceboz Ü, Oral E. “Dietary supplements for treatment of endometriosis: A review.” Acta Biomed, 14, Mar. 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8972862/.
- Gonçalves AV, Barros NF, Bahamondes L. “The Practice of Hatha Yoga for the Treatment of Pain Associated with Endometriosis.” J Altern Complement Med, Jan. 2017. https://pubmed.ncbi.nlm.nih.gov/27869485/.
- Roomaney R, Kagee A. “Coping strategies employed by women with endometriosis in a public health-care setting.” J Health Psychol, Oct. 2016. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4568158/.
- Reis FM, Coutinho LM, Vannuccini S, Luisi S, Petraglia F. “Is Stress a Cause or a Consequence of Endometriosis?” Reprod Sci, Jan. 2020. https://pubmed.ncbi.nlm.nih.gov/32046437/.
- Zollars I, Poirier TI, Pailden J. “Effects of mindfulness meditation on mindfulness, mental well-being, and perceived stress.” Curr Pharm Teach Learn, Oct. 2019. https://pubmed.ncbi.nlm.nih.gov/31685171/.
- Perciavalle V, Blandini M, Fecarotta P, Buscemi A, Di Corrado D, Bertolo L, Fichera F, Coco M. “The role of deep breathing on stress.” Neurol Sci, Mar. 2017. https://pubmed.ncbi.nlm.nih.gov/27995346/.
- Hofmann SG, Gómez AF. “Mindfulness-Based Interventions for Anxiety and Depression.” Psychiatr Clin North Am, Dec. 2017. https://pubmed.ncbi.nlm.nih.gov/29080597/.
- “Can magnesium help to reduce anxiety?” HealthDirect, 13, Jun. 2023. https://www.healthdirect.gov.au/blog/can-magnesium-help-to-reduce-anxiety#:~:text=Magnesium%20may%20help%20to%20control,response%20system%20and%20cortisol%20levels.
- “Coping with Chronic Endometriosis Pain.” Cary OB/GYN. https://www.caryobgyn.com/coping-with-chronic-endometriosis-pain/#:~:text=Make%20heat%20your%20best%20friend,the%20area%20where%20it%20hurts.
- “Complementary and Alternative Therapies for Endometriosis.” Brigham and Wome’s Hospital. https://www.brighamandwomens.org/obgyn/infertility-reproductive-surgery/endometriosis/complimentary-and-alternative-therapies-for-endometriosis.
- “Best Sleeping Positions for Pain.” Cleveland Clinic, 26, May, 2023. https://health.clevelandclinic.org/best-sleeping-positions-for-pain.
Discover how to shrink fibroids naturally at home with diet, lifestyle changes or medical treatments and when to see a doctor.

At 19 weeks pregnant, your baby is growing and you may notice a rounder bump. Learn about fetal development, symptoms, and self-care tips for week 19.
Experiencing bleeding during ovulation? Learn if it’s a sign of pregnancy or normal ovulation bleeding. Discover key differences and when to seek medical advice. Expert insights from Femia.

