Femia > Health Library > Your cycle > Health > Menopause and joint pain: Causes, symptoms, and effective treatments
Menopause and joint pain: Causes, symptoms, and effective treatments
- Updated Feb 11, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
- Menopause joint pain mainly occurs due to reduced estrogen levels in a woman’s body during the perimenopausal and menopausal phases. It also happens because of other factors, like aging, increased weight, and lack of joint movement or physical activity.
- Hormone replacement therapy (HRT) helps replenish low levels of estrogen in the body. In addition, engaging in low-impact exercises, like walking, stretching, and yoga, as well as eating a balanced diet rich in calcium, vitamin D, omega 3, and anti-inflammatory properties, like turmeric, leafy greens, berries, dairy products, fish, and lean meat, can help reduce menopause joint pain and inflammation.
Estrogen is a hormone that maintains our reproductive health and joint tissues. However, when a female reaches menopause, the level of estrogen in her body starts to decline, and low levels of estrogen gradually weaken the joint tissues. Menopause is a phase when you don’t get your menstrual periods for a consecutive 12 months.
Weakening of the joint tissues can contribute to many conditions affecting the joints, like arthritis, degenerative joint, and degenerative disc disease. Although joint pain is common during menopause, it is manageable with the right approaches. Let’s discuss the causes, symptoms, treatment, and prevention of menopause joint pain in detail.
Femia helps you understand your symptoms and when to take action
Can menopause cause joint pain?
Yes, menopause can cause joint pain, but a combination of other factors may also contribute to developing joint pain, like aging, increased weight, and lifestyle factors, like low physical activity and unhealthy diet.
The effects of menopause and other factors on joint health include:
1. Hormonal changes during menopause
The primary hormone responsible for protecting joint tissues and reducing inflammation in the joints is estrogen. But as you reach your 40s, your ovaries start producing less estrogen, which can cause perimenopause joint pain and around the age of 52, the production of estrogen completely stops because of menopause.
Low estrogen levels or lack of estrogen in the body can affect your joints and cause inflammation, leading to pain, swelling, and stiffness.
2. Aging and its effects on joints
With age, our physical and mental health starts to decline. Similarly, the flexibility and movement of our joints become restricted due to changes in tendons and ligaments.
Moreover, cartilage, a flexible connective tissue that cushions the joints and absorbs shock, begins to break because of a lifetime of use. With that, the collagen fibers that keep our skeletal system flexible start to decline as age progresses.
These age-related changes in the joints affect joint lubrication and cause stiffness, loss of motion and flexibility, and joint pain.
3. Weight gain and joint stress
Another factor that affects the joints is increased weight. Excessive fat can increase pressure on the tendons and break the cartilage that cushions the joints, leading to osteoarthritis.
4. Muscle mass decline
Our joints rely on the surrounding muscles, tendons, and ligaments for stability and the muscles help distribute the load of the joints.
The hormonal changes in the body during menopause, effects of aging, and lack of exercise can cause muscle mass decline, weakening joint support. Hence, reduced muscle mass can affect the joints and cause various conditions, like osteoarthritis, degeneration of tendons, and ligament sprains.
5. Bone density reduction
With increased age and low estrogen levels, the bone loses its mineral content, reducing bone density and ability to regrow.
A loss of bone density, a condition known as osteopenia, can progress to osteoporosis and increase the risk of joint and bone fractures.
6. Lifestyle factors
Physical inactivity can also affect joints. It can make your joints stiffer and less flexible, increasing the risks of falls and injuries.
👉Find out more: Can you get pregnant during perimenopause?
What are the symptoms of menopause-related joint pain?
The most commonly affected joints
Menopause can affect the joints of any part of your body due to a decline in estrogen levels. However, the most common joints affected during menopause include the joints of the knees, feet, hips, neck, shoulders, elbows, hands, wrists, and jaws.
The common signs and symptoms of menopause joint pain include:
1. Morning stiffness
One common symptom of menopausal joint pain is morning joint stiffness. It occurs because your joints are still while you sleep, reducing the circulation of synovial fluid that helps lubricate the joints. Moreover, a drop in estrogen levels makes joints more prone to stiffness and increased inflammation.
2. Pain
You may also experience shooting pain or dull aching sensations in your muscles, joints, tendons, and bones. The pain can make it difficult for you to carry out daily activities.
3. Swelling
Another symptom of menopause joint pain is swelling, redness, and warmth around the joints, which are caused by increased inflammation. They may feel tender to touch.
4. Reduced motion
The stiffness, swelling, and pain can decrease the range of motion in your joints, making them less flexible and more difficult to move.
Pain fluctuations throughout the day
Joint pain is a common symptom of menopause, but the pain can fluctuate throughout the day depending on your activities. Excessive physical activity can exacerbate the pain and inflammation, or a lack of motion can make the joints stiff, making it difficult to move.
Taking painkillers can cause menopause joint pain relief for a period of time, but you’ll likely experience pain again when the effects of the medicine wear off.
How to treat menopause joint pain
Let’s move on to the treatment part. Naturally, those experiencing menopause joint pain will want to know how to treat menopause joint pain. Some wonder if treatment is even possible. Well, the answer is, yes, you can treat low estrogen and joint pain with various therapies, natural remedies, and lifestyle modifications, including:
Hormone replacement therapy (HRT) for joint pain
The primary treatment for severe menopausal joint pain is hormone replacement therapy. It is used to treat symptoms of menopause and joint pain, including hot flashes, vaginal discomfort or dryness, and joint and muscle pain.
Hormone replacement therapy (HRT) contains medications to replenish or replace the hormones in the body that are at low levels. To treat severe menopausal symptoms, estrogen is given through hormone replacement therapy, which helps improve low levels of estrogen. Estrogen is normally considered the best hrt for joint pain.
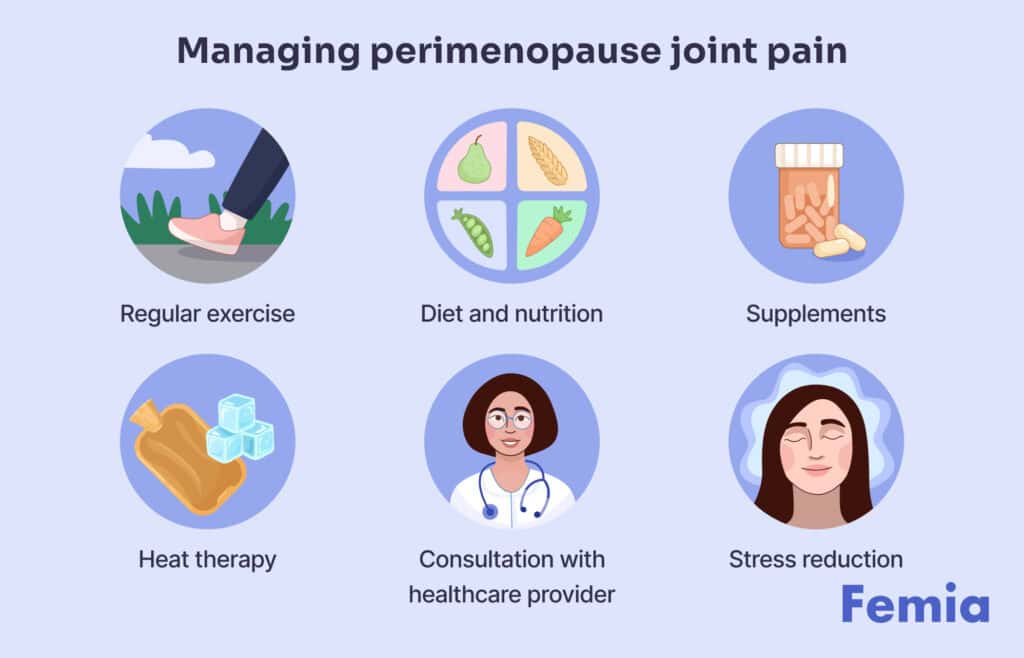
Natural remedies for menopausal joint pain
The primary natural remedy for menopausal joint pain includes focusing on your diet. Incorporate foods in your daily routine that contain anti-inflammatory properties and are rich in calcium and vitamin D.
The foods that are rich in calcium and vitamin D include:
- Yogurt
- Milk
- Egg yolk
- Cheese, especially ricotta cheese.
- Salmon
- Oranges or orange juice
- Mushrooms
- Broccoli
- Sardines, cod liver oil, and canned tuna.
Examples of foods that contain anti-inflammatory properties include:
- Turmeric
- Fruits and vegetables, particularly leafy greens, berries, tomatoes, and bell peppers.
- Fish and lean meats, like mackerel and salmon.
- Nuts and seeds
- Whole grains
The calcium and vitamin D intake will strengthen your bones and joints, and the anti-inflammatory diet will help soothe joint inflammation.
You can also drink herbal teas, like ginger tea, golden turmeric latte, and green tea, as they contain polyphenols and strong anti-inflammatory properties, which can help relieve joint aches and pain.
Exercises for menopause joint pain relief
According to the National Library of Medicine, physical inactivity is a modifiable risk factor for painful and stiff joints in women, which means a significant amount of exercise is required to relieve joint pain.
In menopause, joint pain and low-impact exercises, like walking, yoga, and swimming, are recommended to keep your joints moving and prevent stiffness. High-intensity exercises, like jump squats, mountain climbers, jumping jacks, push-ups, high knees, or others are not recommended in patients with knee pain or osteoarthritis as they may aggravate the pain.
Pain management techniques
Other techniques to manage knee pain during menopause include massaging your knee joints with olive oil, camphor oil, or essential oils, like eucalyptus, lavender, ginger, or rosemary oil, using warm compresses, and taking over-the-counter pain medications like ibuprofen, Tylenol, or diclofenac.
Can supplements help with menopause joint pain?
Yes, supplements can help with joint pain. Still, it is crucial to consult your healthcare provider before starting any supplement, as your doctor can guide you based on your medical history and unique situation.
Certain supplements, like vitamin D and calcium, omega-3 fatty acids, and glucosamine, can help strengthen your bones and joints and support bone density, reducing joint pain.
1. Omega-3 Fatty Acids
The anti-inflammatory properties of omega-3 fatty acids help reduce inflammation associated with menopausal joint pain, making them less stiff and easy to move. The healthy fats in omega-3 fatty acids are typically present in fish oil supplements, which help support overall joint health during menopause.
2. Glucosamine
Glucosamine is a natural compound present in our cartilage, a tissue that cushions the joints. Glucosamine supplements can help increase cartilage and fluid around our joints, improving joint flexibility and reducing pain.
3. Vitamin D and Calcium
Vitamin D and calcium are essential nutrients that are required for maintaining strong bones and joints. Calcium supports bone density, and vitamin D helps the body absorb calcium. Taking vitamin D and calcium supplements during menopause can help reduce the risk of osteoporosis and improve bone and joint health.
Preventing joint pain during menopause
Preventing joint pain during menopause requires making changes in your lifestyle and opting for a healthy routine, including:
1. Maintaining a healthy weight
Increased weight is one of the leading causes of joint pain during menopause as it can put an excessive burden on your joints, break the cartilage that cushions the joints, and make them prone to injuries.
Hence, maintaining a healthy weight is important to reduce pressure on your joints and prevent pain. You can calculate your BMI (body mass index) to measure your body fat based on your height and weight. It is calculated by dividing your weight in kilograms with your height in meters squared. Aim to maintain a healthy BMI, which is between 18.5 and 24.9.
2. Regular exercise
Another factor in preventing joint pain during menopause is keeping your joints moving through regular low-impact exercises, like walking or stretching, like calf raises, arm circles, lunges, squats, and shoulder shrugs, to improve joint flexibility. Regular exercise will improve the range of motion of your joints and reduce pain.
3. Stress management
Uncontrolled and chronic stress can cause joint pain by increasing inflammation in the body and joints. Chronic stress activates your body’s flight and fight response and releases the stress hormone called cortisol.
Cortisol helps regulate the body’s stress response and reduces inflammation. However, prolonged stress and persistent exposure to the cortisol hormone can cause inflammation in the body and joints, leading to joint pain.
Hence, it is crucial to work on stress management by engaging in relaxing activities, like yoga, regular exercise, deep breathing, sound sleep, and participating in things you enjoy.
👉Find out more: Sex after menopause: 10 tips to have orgasms after menopause
When to see a doctor about menopause joint pain
You should visit a doctor regarding your menopausal joint pain if:
- The pain is severe, persistent, and interfering with your daily activities.
- Your joint pain is affecting your movement.
- You are experiencing other symptoms with severe joint pain, like hot flashes, anxiety, depression, and tenderness and swelling in the joints.
Your joint pain may not necessarily occur from menopause, so it is essential to go for other diagnostic tests, like a CT scan or MRI of your joints, to rule out other conditions or causes of joint pain.
Femia helps you understand your symptoms and when to take action
Questions from the Femia community
Can menopause joint pain feel like arthritis?
Yes, menopausal joint pain commonly feels like arthritis, as both conditions can involve pain, stiffness, and swelling in the joints. Menopause often causes arthritis because of low estrogen levels.
How long will my menopause joint pain last?
The duration and intensity of menopause joint pain can vary from person to person, as joint pain can occur from a combination of different factors, like overusing joints, aging, injury, daily exercise and dietary habits, and menopause.
Some individuals may experience menopausal joint pain over a few years while their hormonal levels stabilize. Some people may experience it for a long time and may require treatments to manage their condition, like joint replacement and hormone replacement therapy.
Can menopause joint pain affect my sleep?
Yes, menopausal joint pain can affect your sleep quality as pain can cause disturbances while sleeping, especially if it occurs with other menopausal symptoms, like night sweats, hot flashes, anxiety, and depression. Moreover, if your bedding doesn't provide enough support to the joints, it can cause pain while sleeping.
Are my hot flashes connected to joint pain?
Both hot flashes and joint pain are the symptoms of menopause and are caused by a decline in estrogen levels. Although the symptoms are not connected to each other, hot flashes can make you feel increased discomfort in the joints.
The bottom line
Menopause joint pain is common, but it is manageable with a combination of natural and medical approaches. Mild joint pain can be reduced with low-impact exercises, a balanced diet, and over-the-counter anti-inflammatory medicines, like ibuprofen and diclofenac sodium.
However, if you experience intense joint pain and persistent symptoms, it is ideal to consult a healthcare provider for estrogen replacement therapy or other treatments, depending on your condition.
References
- “Osteopenia.” Cleveland Clinic, 1 Oct. 2024, my.clevelandclinic.org/health/diseases/21855-osteopenia.
- “Symptoms.” NHS, 19 Sept. 2024, www.nhs.uk/conditions/menopause/symptoms.
- “Treatment.” NHS, 21 July 2023, www.nhs.uk/conditions/menopause/treatment.
- Heesch, Kristiann C., et al. “Relationship Between Physical Activity and Stiff or Painful Joints in Mid-aged Women and Older Women: A 3-year Prospective Study.” Arthritis Research & Therapy, vol. 9, no. 2, Jan. 2007, p. R34. https://doi.org/10.1186/ar2154.
- Messier, Stephen P., et al. “Effect of High-Intensity Strength Training on Knee Pain and Knee Joint Compressive Forces Among Adults With Knee Osteoarthritis.” JAMA, vol. 325, no. 7, Feb. 2021, p. 646. https://doi.org/10.1001/jama.2021.0411.
- Cordingley, Dean M., and Stephen M. Cornish. “Omega-3 Fatty Acids for the Management of Osteoarthritis: A Narrative Review.” Nutrients, vol. 14, no. 16, Aug. 2022, p. 3362. https://doi.org/10.3390/nu14163362.
- “Cortisol.” Cleveland Clinic, 1 May 2024, my.clevelandclinic.org/health/articles/22187-cortisol.

Learn about the process of implantation, discover the early signs, such as implantation bleeding and cramping, and how the hormone hCG becomes detectable soon after.

Explore possible symptoms at 7 days past ovulation (7 DPO), including mild cramping and cervical mucus changes. Understand when a pregnancy test may be accurate. Expert advice from Femia.

There are lots of different types of vibrators and it can be difficult to choose. Find out the best vibrator for women and different types of sex toys.