Femia > Health Library > Your cycle > Health > PCOS Belly: Why’s and how’s
PCOS Belly: Why’s and how’s

- Updated Mar 2, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
Polycystic ovary syndrome (PCOS) causes symptoms like insulin resistance, hormonal imbalance, and weight gain, often resulting in a “PCOS belly,” a colloquial term that has been popularized in social media. The fat is concentrated around the abdomen and for females with insulin resistance, is harder to lose because of hormonal fluctuations and high levels of insulin. The dietary and lifestyle changes, as well as specific medications prescribed by doctors, can help manage weight loss.
Polycystic ovary syndrome (also known as PCOS) is one of the most common endocrine diseases among women. According to the World Health Organization, PCOS affects 8–13% of all women of reproductive age. And, as you may already know, this disease also causes higher risks of infertility among women.
👉 Find out more: Best age to get pregnant with PCOS: When to start and what you need to know
Symptoms vary, but the most common ones are insulin resistance, diabetes, reproductive hormone imbalance, missed periods, and weight gain. Notably, the last symptom isn’t only about weight in general.
PCOS causes a phenomenon known as “PCOS belly”—an apple-shaped belly with a prominent fat pad around the middle of the waist. Let’s explore everything you may want to know about this PCOS symptom and how to treat it.
What is PCOS belly?
PCOS belly is characterized as an accumulation of abdominal fat in women diagnosed with PCOS. Since PCOS causes hormonal changes and weight gain, women may have increased body fat and weight gain all around the body.
But, in some cases, there is a higher chance of fat concentrated on the belly that is hard to shed. Even when having an ideal body mass index, PCOS makes it much harder to get rid of belly fat.
According to Dr. Trish Kahawita, two main reasons for PCOS belly are hormonal fluctuations and insulin resistance.
PCOS makes it harder for the body to properly use the hormone insulin, which is supposed to help convert sugars and starches from foods into energy. Insulin resistance causes insulin and sugar to build up in the bloodstream and stored as fat instead of being converted into energy.
These high insulin levels in the bloodstream increase the production of male sex hormones called androgens. High levels of this hormone often lead to symptoms like excessive body hair growth, acne, irregular periods, and weight gain.
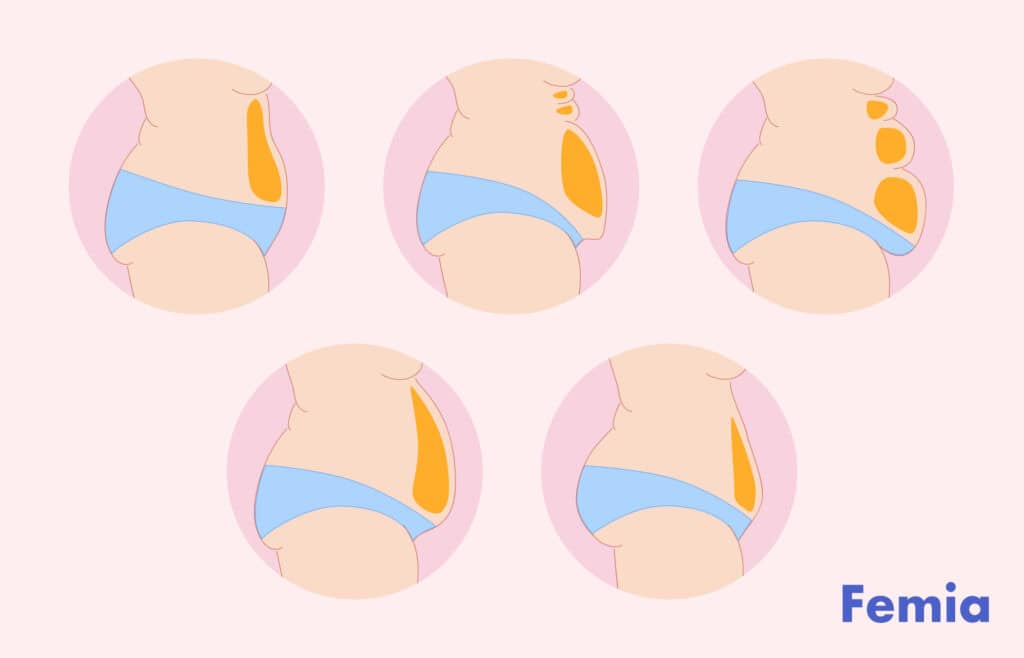
PCOS belly shape: Is it different, and how?
Even though you may know what a PCOS belly looks like, you may still wonder whether it is possible to confuse it with just obesity or even a pregnant belly. Let’s learn the differences:
PCOS Belly Shape vs. General Obesity
PCOS belly shape:
- Fat distribution: PCOS causes an “apple-shaped” body, with weight gain that is concentrated around the abdomen while the rest of the body might be without significant changes.
- Appearance: The belly may appear more distended and firm compared to other types of fat distribution.
- Underlying causes: Hormonal imbalance, insulin resistance, and metabolic syndrome are key reasons.
General obesity belly shape:
- Fat distribution: fat is more evenly distributed throughout the body, though it still can be concentrated in areas like the abdomen, hips, and thighs. The rest of the body also has visible weight gain changes.
- Appearance: the fat in general obesity is often softer and more evenly spread across different parts of the body.
- Underlying causes: overeating, lack of physical activity, genetics, and related metabolic conditions.
PCOS Belly vs Pregnant Belly: visual differences
PCOS belly:
- Shape and firmness: The belly is generally more round and firm due to the central accumulation of fat. It does not grow or change shape significantly over a short period.
- Consistency: firmness is caused by fat and sometimes bloating rather than a growing uterus or fluid accumulation associated with pregnancy.
Pregnant belly:
- Shape and firmness: The pregnant belly is more protruded and can be softer, depending on the stage of pregnancy. The belly grows and changes over the course of the pregnancy.
- Consistency: the belly is firm because of the growing fetus, uterus, and amniotic fluid.
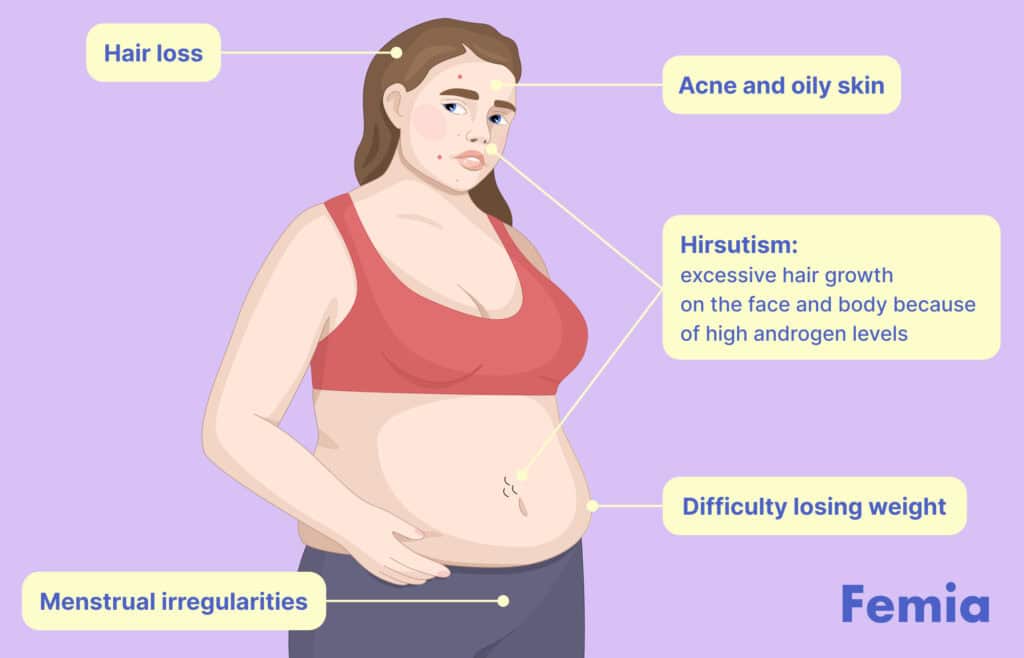
Signs and symptoms: how to distinguish PCOS belly?
PCOS-related weight gain:
- Menstrual irregularities: women struggling with PCOS often experience irregular menstrual cycles, like missed and prolonged periods.
- Hirsutism: excessive hair growth on the face and body because of high androgen levels.
- Acne and oily skin: hormonal imbalances can lead to skin issues.
- Hair loss: thin hair and male-pattern baldness may also be a sign.
- Difficulty losing weight: insulin resistance and metabolic issues make losing weight challenging.
Pregnancy:
- Missed periods: one of the biggest symptoms of pregnancy is the absence of menstrual periods.
- Morning sickness: pregnant women often experience nausea and vomiting. It is a common sign of early pregnancy.
- Breast changes: tender, swollen breasts with darkened areolas.
- Fatigue: increased tiredness due to hormonal changes. Please note that this symptom is also linked to other conditions, so consulting a healthcare provider is a must, especially when it comes to extreme fatigue without any other pregnancy symptoms.
- Frequent urination: as the uterus grows, it puts pressure on the bladder. Similar to fatigue, this can also be a symptom of several diseases if noticed without any other signs of pregnancy, and it’s important to consult a doctor in this case.
If there are any concerns regarding unusual weight gain or changes in body shape, it is essential to consult with a doctor for accurate diagnosis and appropriate treatment.
PCOS body shape: what else to know?
Since PCOS-related weight gain is triggered by male hormones, fat is usually concentrated on the belly. That is where men traditionally tend to gain weight. So, instead of having more pear shape, women with PCOS usually have a so-called “apple” body shape.
Key changes in the body shape experienced by women with PCOS are:
- Shorter extremities when compared to those without the disease, according to the research of Vilnius University;
- Central fat distribution;
- Visceral fat;
- Increased waist circumference.
👉Find out more: PCOS supplements: Best options for weight loss, fertility, and symptom management
Managing PCOS belly fat: 3 best practices
Below, you can explore some of the general recommendations that may help to assist in losing belly fat when being diagnosed with PCOS. However, note that only a healthcare provider can create a tailored treatment plan for your specific health circumstances.
1. Dietary changes
- Focus on whole foods that are high in fiber, lean proteins, and healthy fats. Try to avoid or at least minimize sugar, processed foods, and excessive carbohydrates.
- Consider balancing your meals with proteins, carbohydrates, and fats. This may mean one quarter for protein, one for complex carbohydrates, and two quarters for vegetables.
- Try to eat 4–5 smaller meals a day rather than 2–3 large ones. This helps avoid unhealthy cravings and avoid overeating.
- Drink enough water to help digestion, reduce bloating, and support overall well-being.
👉 Find out more: Enhancing fertility naturally: A guide to fertility supplements and foods for women
2. Include more physical activity
Cardio exercises:
- High-Intensity Interval Training (HIIT): 30 seconds of sprinting followed by 1 minute of walking, which is repeated for 20–30 minutes.
- Brisk walking: aim for at least 30 minutes of brisk walking every day.
- Cycling: incorporate intervals by alternating between moderate and intense paces.
- Swimming: try swimming at least twice a week.
- Dancing: use dance workouts that elevate your heart rate and engage various muscle groups.
Strength training exercises:
- Planks: hold for 30–60 seconds, rest, and repeat 3–5 times.
- Leg raises: lie on your back, lift your legs to a 90-degree angle, lower them slowly without touching the ground, and repeat for 15–20 reps.
- Bicycle crunches: lie on your back, lift your legs, and alternate bending each leg while bringing your knee toward your chest in a pedaling motion, bringing your elbow to the opposite knee at the same time.
3. Medical treatments
Medical treatments should only be prescribed by a healthcare professional; the information below is only for educational purposes. Here are some of the treatments that doctors may consider:
- Insulin-sensitizing medications: help lower insulin levels and reduce symptoms like weight gain and irregular cycles.
- Hormonal birth control: help regulate menstrual cycles, reducing androgen levels.
- Anti-androgen medications: this medication helps to reduce androgen levels, which can decrease symptoms such as excess hair growth and acne and potentially assist in weight management.
- Weight loss medications: can help with weight loss by reducing the absorption of dietary fat.
Questions from the Femia community
Do all women with PCOS have a PCOS belly?
The short answer is “no.” While belly fat is a common symptom of PCOS, not all women with the disease will have significant abdominal fat.
Can Ozempic help with PCOS belly?
Ozempic is not specifically approved for PCOS. However, healthcare professionals sometimes consider this drug because of its positive effects on weight loss and insulin resistance.
Is surgery an option for PCOS belly fat?
Surgery might be an option, but it is often considered only after dietary management, lifestyle changes, and medications. If these don't work, consult healthcare professionals for more options, including surgery.
The bottom line
Recognizing PCOS belly is crucial for effective management of the condition. Hormonal imbalances and insulin resistance are primary reasons for abdominal fat accumulation in women with PCOS.
Treatment and symptom management involves a combination of lifestyle modifications, including a balanced diet, regular exercise, and medical interventions prescribed by healthcare providers. Consulting with healthcare professionals is essential to get a personalized treatment plan.
References
- World Health Organization. “Polycystic Ovary Syndrome.” Www.who.int, 28 June 2023, www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome#:~:text=Polycystic%20ovary%20syndrome%20(PCOS)%20affects.
- Centers for Disease Control and Prevention. “PCOS (Polycystic Ovary Syndrome) and Diabetes.” Centers for Disease Control and Prevention, 12 Aug. 2022, www.cdc.gov/diabetes/basics/pcos.html.
- Justyna Jurczewska, et al. “Abdominal Obesity in Women with Polycystic Ovary Syndrome and Its Relationship with Diet, Physical Activity and Insulin Resistance: A Pilot Study.” Nutrients, vol. 15, no. 16, 20 Aug. 2023, pp. 3652–3652, https://doi.org/10.3390/nu15163652. Accessed 23 Sept. 2023.
- “Fertility Specialists.” Southern California Reproductive Center, www.scrcivf.com/doctors/shahin-ghadir/. Accessed 17 July 2024.
- Purwar, Ananya, and Shailesh Nagpure. “Insulin Resistance in Polycystic Ovarian Syndrome.” Cureus, vol. 14, no. 10, 16 Oct. 2022, https://doi.org/10.7759/cureus.30351.
- Ye, Wenting, et al. “The Role of Androgen and Its Related Signals in PCOS.” Journal of Cellular and Molecular Medicine, vol. 25, no. 4, 23 Dec. 2020, pp. 1825–1837, https://doi.org/10.1111/jcmm.16205.
- Rasquin Leon, Lorena I., et al. “Polycystic Ovarian Disease.” PubMed, StatPearls Publishing, 2023, www.ncbi.nlm.nih.gov/books/NBK459251/#:~:text=Many%20features%20of%20PCOS%20are.
- Rasquin Leon, Lorena I., et al. “Polycystic Ovarian Disease.” PubMed, StatPearls Publishing, 2023, www.ncbi.nlm.nih.gov/books/NBK459251/#:~:text=Many%20features%20of%20PCOS%20are.
- Carmina, Enrico, et al. “Female Adult Acne and Androgen Excess: A Report from the Multidisciplinary Androgen Excess and PCOS Committee.” Journal of the Endocrine Society, vol. 6, no. 3, 6 Feb. 2022, www.ncbi.nlm.nih.gov/pmc/articles/PMC8826298/, https://doi.org/10.1210/jendso/bvac003.
- Prasad, Sonya, et al. “Polycystic Ovary Syndrome in Patients with Hair Thinning.” Journal of the American Academy of Dermatology, vol. 83, no. 1, July 2020, pp. 260–261, www.ncbi.nlm.nih.gov/pmc/articles/PMC8291365/, https://doi.org/10.1016/j.jaad.2020.01.075.
- “Nausea and Vomiting in Pregnancy (NVP).” PubMed, Organization of Teratology Information Specialists (OTIS), 1994, www.ncbi.nlm.nih.gov/books/NBK582541/#:~:text=NVP%20or%20. Accessed 17 July 2024.
- Mortazavi, Forough, and Fateme Borzoee. “Fatigue in Pregnancy: The Validity and Reliability of the Farsi Multidimensional Assessment of Fatigue Scale.” Sultan Qaboos University Medical Journal [SQUMJ], vol. 19, no. 1, 30 May 2019, p. 44, https://doi.org/10.18295/squmj.2019.19.01.009.
- Bello, F.A., and A.O Odeku. “POLYCYSTIC OVARIES: A COMMON FEATURE in TRANSVAGINAL SCANS of GYNAECOLOGICAL PATIENTS.” Annals of Ibadan Postgraduate Medicine, vol. 13, no. 2, 1 Dec. 2015, pp. 108–109, www.ncbi.nlm.nih.gov/pmc/articles/PMC4853876/.
- Zabuliene, L., et al. “Skeletal Frame Size in Females with Polycystic Ovary Syndrome.” Endocrine Abstracts, vol. 29, 1 May 2012, www.endocrine-abstracts.org/ea/0029/ea0029p947#:~:text=Conclusions%3A%20Women%20with%20PCOS%20have. Accessed 17 July 2024.
- Xenou, Maria, and Kleanthi Gourounti. “Dietary Patterns and Polycystic Ovary Syndrome: A Systematic Review.” Maedica – a Journal of Clinical Medicine, vol. 16, no. 3, 15 Sept. 2021, https://doi.org/10.26574/maedica.2020.16.3.516.
- Lord, J M, et al. “Insulin-Sensitising Drugs (Metformin, Troglitazone, Rosiglitazone, Pioglitazone, D-Chiro-Inositol) for Polycystic Ovary Syndrome.” The Cochrane Database of Systematic Reviews, no. 3, 2003, p. CD003053, www.ncbi.nlm.nih.gov/pubmed/12917943/, https://doi.org/10.1002/14651858.CD003053. Accessed 2 Jan. 2020.
- Melo, Anderson, et al. “Hormonal Contraception in Women with Polycystic Ovary Syndrome: Choices, Challenges, and Noncontraceptive Benefits.” Open Access Journal of Contraception, vol. Volume 8, no. 8, Feb. 2017, pp. 13–23, https://doi.org/10.2147/oajc.s85543.
- Rittmaster, Roger S. “ANTIANDROGEN TREATMENT of POLYCYSTIC OVARY SYNDROME.” Endocrinology and Metabolism Clinics of North America, vol. 28, no. 2, June 1999, pp. 409–421, https://doi.org/10.1016/s0889-8529(05)70077-3. Accessed 3 Feb. 2021.
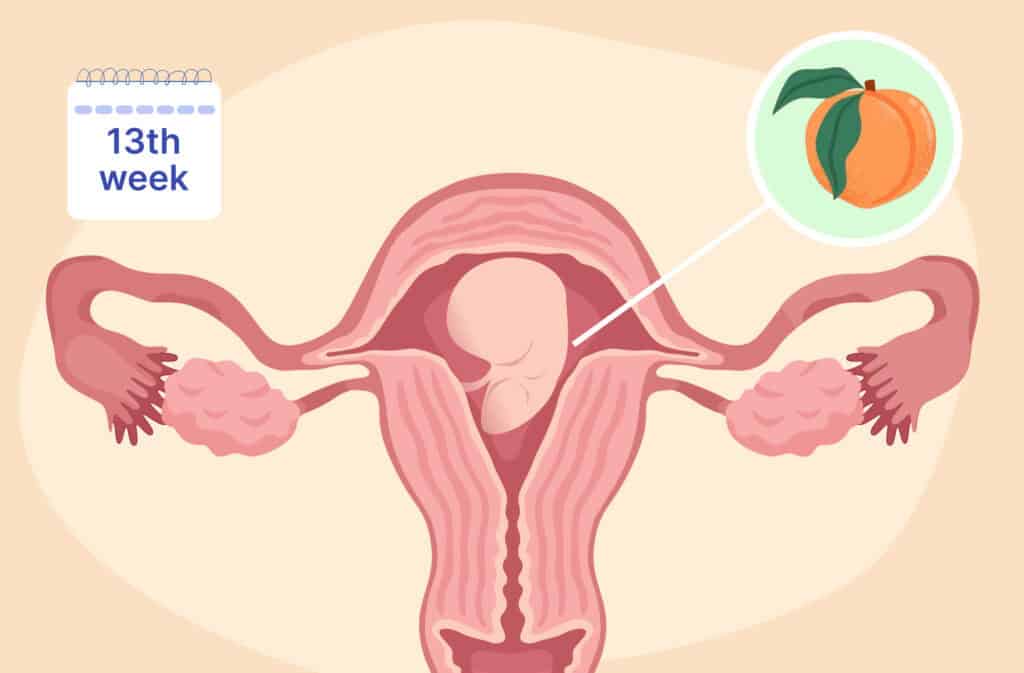
Discover what happens at 13 weeks pregnant, from baby’s development and bump changes to ultrasound insights and common symptoms.

Discover key signs your body is ready for pregnancy. Learn how to know if you’re fertile enough to get pregnant: physical indicators, medical tests, etc. Expert advice from Femia.
Kansas has filed a lawsuit against Pfizer, alleging misinformation about its COVID-19 vaccine’s safety and effectiveness, including during pregnancy. Learn more about the claims, evidence, and implications.

