Femia > Health Library > Your cycle > Health > Why am I not ovulating but still having periods? Understanding anovulation
Why am I not ovulating but still having periods? Understanding anovulation

- Updated Feb 11, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
- If your ovaries fail to release an egg, ovulation hasn’t occurred, and you can’t get pregnant during that cycle.
- Anovulation can cause bleeding resembling a period.
- Anovulation can be caused by a variety of conditions, including stress, polycystic ovary syndrome (PCOS), thyroid issues, and perimenopause.
Without ovulation, you can’t conceive naturally during that cycle.
Anovulation occurs when the ovary fails to release an egg. When this happens, there is no chance of conceiving during that cycle. Some women miss periods during anovulation, which offers a clue that something might be amiss.
However, you can bleed after an anovulatory cycle; though it isn’t technically a period, it can be easily mistaken for one.
Femia helps millions of women track their cycles and fertile windows
What is ovulation?
Ovulation normally occurs once during each menstrual cycle, usually around its midpoint (day 14 if you have a 28-day cycle). During ovulation, an egg is released from an ovary and travels down the fallopian tube towards the uterus. The egg can survive for up to 24 hours.
Your fertile window begins five days before ovulation (because sperm can survive up to five days inside your body waiting for an egg) and finishes the day after ovulation occurs. If sperm reaches the egg during this fertile window, you might conceive.
Hormonal fluctuations during the ovulation phase can lead to various physical and emotional symptoms. The most common include:
- Breast tenderness
- Bloating
- Changes in cervical position and firmness
- Increased libido
- Heightened senses (such as smell, sight, or taste)
- Changes in appetite
- Mood swings
Can you have a period without ovulating?
Technically, you can’t menstruate without ovulating first. However, changing hormone levels mean many women experience bleeding that they (understandably) mistake for a regular period. This bleeding is often referred to as a withdrawal bleed.
An AUB may be lighter or heavier than your regular period, which may be a hint that it’s not a run-of-the-mill cycle. These bleeds can also be irregularly timed, so tracking your cycles can help you notice if it occurs and give you a better idea of what’s happening in your body.
👉Find out more: PMS vs pregnancy symptoms: How to tell the difference?
Why am I not ovulating but having periods?
You’re not having a true period, though it may seem that way. If you aren’t ovulating, what you’re experiencing are withdrawal bleeds caused by hormonal changes. You must ovulate to have a period, which is why the bleeds you have when on the contraceptive pill are described as withdrawal bleeds rather than periods.
So, if you’re wondering “can you have a period and not ovulate?”, the answer is technically no—but you can have a bleed that resembles one.
What is anovulation?
Anovulation occurs when the ovaries fail to release an egg for ovulation. Instead of releasing a mature egg, the eggs are reabsorbed into the body.
Anovulation can be a temporary condition—if it lasts for over a year, it is known as chronic anovulation, which is a common cause of infertility. The good news is that it’s usually a treatable condition, and the sooner you get a diagnosis, the sooner you can start treatment.
Causes of anovulation
Anovulation can be caused by several factors:
- Hormonal imbalances: Imbalances in estrogen, progesterone, FSH, and LH can disrupt the ovulation process and menstrual cycle.
- Polycystic ovary syndrome (PCOS): A common hormonal disorder that causes high androgen levels, irregular periods, and cysts on the ovaries, often resulting in anovulation.
- Thyroid disorders: Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can interfere with ovulation by affecting hormone regulation.
- Excessive physical or emotional stress: High stress levels can disturb the hormonal balance necessary for ovulation.
- Being underweight or overweight: Extreme body weight can affect hormone production and disrupt ovulation.
- Premature ovarian failure (POF): This occurs when the ovaries stop functioning before the age of 40, leading to anovulation and infertility.
- Certain medications: Medications like hormonal contraceptives and chemotherapy drugs can impact ovulation either temporarily or permanently.
Symptoms of anovulatory cycle
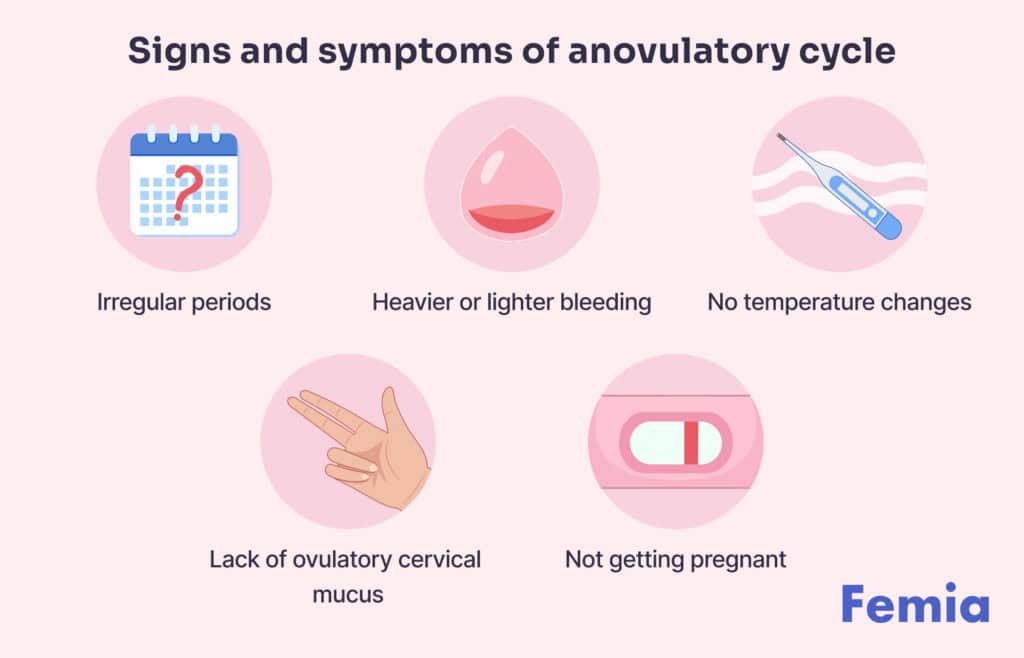
Being aware of the signs of ovulation and tracking your menstrual cycle can help you identify potential signs of anovulation. It’s important to understand that having a period doesn’t always indicate ovulation. Here are some common signs and symptoms of anovulation:
Irregular periods: If your cycle length frequently changes, this could be a sign of anovulation. While the typical cycle is 28 days, variations of a few days shorter or longer are common, but inconsistent cycles may indicate an issue.
Heavy or light periods: A heavy period involves losing more than 16 teaspoons (80 mL) of blood or lasting longer than seven days. A light period has less than 4 teaspoons (20 mL) of blood over the course of your cycle. If you consistently fill a pad every hour for several hours, it’s considered heavy.
Missed periods (amenorrhea): Missing one or more periods without pregnancy may be a clear indicator of anovulation.
Lack of egg-white cervical mucus: Around ovulation, cervical mucus should resemble raw egg whites—clear, stretchy, and slippery. If you don’t experience this, you may not be ovulating.
Irregular basal body temperature: Your basal body temperature, measured first thing in the morning before you get out of bed, typically rises slightly after ovulation. If there’s no noticeable temperature change, it might suggest anovulation.
Recognizing these signs can help you determine whether you’re ovulating or experiencing anovulation, so you can seek appropriate advice and care.
How anovulation is diagnosed
When you attend your consultation, your doctor will take a medical history and ask questions to learn more about your fertility. They may ask whether you’ve been tracking ovulation signs such as basal body temperature and cervical mucus. If you haven’t been tracking these, they may ask you to do so from now on.
Your doctor might take a few steps to understand what’s happening with your body:
- Blood tests. They may check your hormone levels to see if there’s an imbalance that could be affecting ovulation.
- Ultrasound exam. This allows them to look at your pelvic organs, checking for signs of ovulation and any potential issues.
- Progesterone challenge. Your doctor might suggest this test to check how your body responds to progesterone. Here’s how it works:
- You’ll take progesterone for a set number of days.
- If you have a “withdrawal bleed” (similar to a period) after stopping the progesterone, it suggests your uterine lining is building up but not shedding regularly.
- If you don’t have bleeding, it might indicate lower estrogen levels or other issues.
This combination of tests helps your doctor get a clearer picture of what might be affecting your cycles and fertility.
Tracking ovulation and menstrual patterns
Tracking ovulation is key to understanding your fertility window and optimizing your chances of conception. There are several methods available to track ovulation, each offering valuable insights:
Basal body temperature (BBT) tracking: Monitoring your body temperature every morning before getting out of bed can help you identify the slight increase that happens after ovulation.
Ovulation predictor kits (OPKs): These tests detect the surge in luteinizing hormone (LH), which occurs right before ovulation, helping you pinpoint your most fertile days.
Cervical mucus monitoring: Tracking changes in your cervical mucus throughout your cycle can reveal the most fertile days, as it becomes clear, slippery, and stretchy around ovulation.
Calendar method: By tracking the length of your menstrual cycles over several months, you can estimate your ovulation window.
Period tracker app: Apps like Femia help to track ovulation and menstrual patterns, offering personalized insights and recommendations based on your unique cycle.
Using a combination of these methods can help you more accurately track ovulation and improve your chances of conception.
👉Find out more: Can you get pregnant on your period? Understanding the odds and timing
Treatment options for anovulation
Treatment options for anovulation can vary depending on the underlying cause of the condition, but the goal is to restore ovulation and improve fertility. Here are the main treatment options commonly used:
Lifestyle modifications: If anovulation is caused by factors like stress, poor nutrition, or being overweight or underweight, making lifestyle changes such as improving diet, increasing physical activity, and managing stress can help restore ovulation.
Medications to induce ovulation:
- Clomiphene citrate: This is one of the most common medications used to induce ovulation by stimulating the release of hormones necessary for ovulation.
- Letrozole: This drug, often used for breast cancer treatment, can also stimulate ovulation and may be an alternative to clomiphene for women who do not respond to it.
- Gonadotropins: These injectable hormones, which include FSH and LH, can stimulate the ovaries directly to produce eggs. They are often used when clomiphene or letrozole does not work.
Metformin: For women with PCOS and insulin resistance, metformin can help regulate insulin levels and encourage ovulation. It is often used in combination with other treatments.
Surgery:
- Ovarian drilling: In cases of PCOS, when other treatments are unsuccessful, a surgical procedure called ovarian drilling can be used to stimulate ovulation by making small holes in the ovaries with a laser or electrical current.
Intrauterine insemination (IUI): For women who have issues with sperm motility or low sperm count, IUI can be paired with ovulation-inducing medications to increase the chances of sperm reaching the egg.
In vitro fertilization (IVF): If other treatments do not work, IVF can be an option. In this procedure, eggs are retrieved from the ovaries, fertilized in a lab, and the embryos are transferred to the uterus.
Thyroid hormone therapy: For women with hypothyroidism or hyperthyroidism, treating the thyroid condition can help restore ovulation.
Corticosteroids: In cases where the anovulation is caused by autoimmune diseases or inflammatory conditions, corticosteroids can be prescribed to reduce inflammation and restore ovulation.
It’s important to consult with a healthcare provider to determine the appropriate treatment plan based on the underlying cause of anovulation. A tailored approach will provide the best chances of restoring fertility.
How does anovulation affect fertility?
If you don’t ovulate, you can’t get pregnant, so anovulation is may not be the news you want to hear. It can be distressing to hear you’re not ovulating when you are trying for a baby, but you’ll be relieved to hear there are treatment options available to you.
If you think you might be having anovulatory cycles, you should consult with your OBGYN for advice. There are lifestyle changes you can make to treat anovulation, plus medication options if those don’t work. Your doctor will want to determine the cause of your anovulatory cycles before using medication.
👉Find out more: How to recognize signs of high fertility in a woman: A detailed guide
What happens to your eggs if you don’t ovulate?
If you’re wondering what happens to your eggs if you don’t ovulate, you might be surprised to hear you usually lose more than one egg monthly. While only one egg matures and is released during ovulation, around 15–20 eggs are activated each cycle. The winning egg matures and gets released during ovulation, and the body reabsorbs the remaining follicles in a process known as atresia.
While the idea of losing eggs might sound scary, especially if you suffer from chronic anovulation, it’s important to remember you are born with more than enough eggs. Your egg count when you born is around two million eggs. You lose around 1,000 per month to cell damage but will still have plenty of eggs left over.
Chronic anovulation isn’t good news when you’re trying to conceive, but once you have a diagnosis, you can start treatment to kickstart ovulation again.
If ovulation tests negative, can I still get pregnant?
Testing timing: If you take the ovulation test at the wrong time of day or too early in your cycle, you might miss the LH surge. Ovulation can sometimes occur outside the expected window, so testing multiple times a day during your fertile window can increase the accuracy of results.
Irregular cycles: If you have irregular menstrual cycles, predicting ovulation can be tricky. Some women may not have a typical LH surge or ovulate later or earlier than expected.
Low LH surge: In some cases, you might experience a subtle or low LH surge, which might not be detected by an ovulation test, but you can still ovulate and potentially get pregnant.
Other factors: Other factors, like stress, hormone imbalances, or underlying health conditions, can also impact ovulation, potentially leading to a negative ovulation test result even when ovulation is happening.
While a negative ovulation test does not guarantee that conception is impossible, it’s helpful to track other signs of ovulation, such as cervical mucus changes and basal body temperature, and consider discussing your fertility with a healthcare provider if you are struggling to conceive.
Femia helps millions of women track their cycles and fertile windows
Questions from Femia community
Can I still get pregnant during an anovulatory cycle?
No, it’s not possible to conceive during an anovulatory cycle. Without ovulation, there is no egg for the sperm to fertilize; therefore, pregnancy can’t occur. It’s worth tracking your symptoms, such as cervical mucus and basal body temperature, throughout your cycle to identify any potential signs of skipped ovulation.
What’s the difference between a regular period and bleeding during an anovulatory cycle?
The bleeding following anovulatory cycles tricks some women into thinking they’re menstruating. Changing hormone levels cause an irregular bleed, which isn’t technically a period but may happen around the time women are expecting their period. This bleed might be heavier or lighter than a regular period. These bleeds are often irregularly timed, so if you have irregular periods, this could actually be a sign of anovulatory cycles.
Does anovulation mean infertility?
Anovulation can make it difficult to conceive, but it doesn’t always mean infertility. Many women can become pregnant once ovulation is restored with treatment or lifestyle changes. Underlying conditions like PCOS can also be managed to help restore fertility.
How to tell if you're not ovulating?
Signs of anovulation include irregular periods, lack of cervical mucus changes, no temperature rise after ovulation, and missed periods. Negative ovulation tests throughout the cycle can also indicate anovulation. If you suspect you’re not ovulating, consult with a healthcare provider for further evaluation and treatment options.
The bottom line
Anovulation is a common condition that can impact fertility. Though this might sound scary, the good news is there are treatments available. Understanding your cycle and tracking bodily changes throughout the month can help you identify anovulation early. Your doctor will then be able to work with you to figure out the cause and recommend treatment options.
Anovulatory cycles can be linked to weight issues, stress, and excessive exercise, so there are lifestyle changes you can make to improve your reproductive health. Your doctor will look for underlying health conditions and treat any that could be preventing ovulation. There are also medications available that can trigger ovulation, which your doctor may suggest to help you conceive.
While reading about anovulation might sound scary when you’re trying for a baby, having a diagnosis is a good thing. Once you have a diagnosis, you have treatment options available to help you conceive.
References
- Hamilton-Fairley, Diana, and Alison Taylor. “Anovulation.” BMJ (Clinical research ed.) vol. 327,7414 (2003): 546-9. doi:10.1136/bmj.327.7414.546 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC192851/.
- Hsiu-Wei Su et al. “Detection of ovulation, a review of currently available methods.” Bioengineering & Translational Medicine (2017) https://doi.org/10.1002/btm2.10058.
- Holesh JE, Bass AN, Lord M. Physiology, Ovulation. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441996/.
- Jones K, Sung S. Anovulatory Bleeding. [Updated 2023 Jul 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549773/.
- Rolaki, Alexandra et al. “Novel trends in follicular development, atresia and corpus luteum regression: a role for apoptosis.” Reproductive biomedicine online vol. 11,1 (2005): 93-103. doi:10.1016/s1472-6483(10)61304-1 https://pubmed.ncbi.nlm.nih.gov/16102296/#:~:text=During%20atresia%20and%20luteolysis%2C%20granulosa,apoptotic%20process%20prior%20the%20ovulation.
How long does IVF take from the first appointment to a successful pregnancy? Read a complete guide to the IVF process and timeline to learn what to expect.
At 23 weeks pregnant, your baby is about the size of a grapefruit. Explore symptoms, baby movements, and expert tips for managing week 23.

Discover what happens at 30 weeks pregnant, from baby’s development and weight gain tips to symptoms and labor prep.

