Femia > Health Library > Your cycle > Ureaplasma in females: Symptoms, diagnosis, and partner transmission
Ureaplasma in females: Symptoms, diagnosis, and partner transmission

- Updated Mar 1, 2025
- Published
CRAFTED BY HUMAN
Crafted by human At Femia, we provide accurate and up-to-date information at every stage of your journey, from trying to conceive, pregnancy and postnatal support. All content is created by a real person based on in-depth research and own professional experience. Femia ensures that you will receive expert advice, strict accuracy and a personalized approach from our authors/medical experts. Learn more about our editorial policy.
FACT CHECKED
Fact checked At Femia Health, we maintain the highest standards of editorial excellence in delivering content focused on helping you conceive, guiding you through pregnancy, and supporting you postpartum. Explore our content review principles to learn how we ensure the accuracy and quality of our health and lifestyle tips for every stage of your journey.
Common ureaplasma symptoms may include painful urination, vaginal discharge, itching, and others, though the infection can also run symptom-free. Although it is often identified as an STI, it can be detected in healthy and sexually inactive humans. Timely testing and treatment are important to mitigate health risks and prevent reinfection.
Ureaplasma is among the smallest and most prevalent genital bacteria found in the urinary and reproductive tract. Due to its common nature and simple transmission, ureaplasma is found in many people, both females and males. It can be transmitted between partners during sex and often doesn’t cause physical symptoms, so it might go unnoticed, which makes it an important thing to be aware of.
This guide will explain the definition and symptoms of ureaplasma in females as well as other factors worth knowing to help you understand this condition.
What is ureaplasma?
Ureaplasma species are among the most prevalent genital bacterium in both men and women. These bacteria fall into the Mollicutes class—they are distinguished by the absence of a cell wall, which makes them very small. Ureaplasma species are tiny, free-living, self-replicating microorganisms found in the urinary and reproductive tracts.
There are two types of this bacteria:
- Ureaplasma urealyticum. Often a type of sexually transmitted infection (STI) and is associated with Bacterial Vaginosis.
- Ureaplasma parvum. Often identified as a commensal in the uterus and a natural part of the microbiome in healthy women of reproductive age.
Knowing about this bacteria and its symptoms is pivotal due to its prevalence in the natural female microbiome. Ureaplasma spp. is reported in 40%–80% of clinically healthy women in the USA.
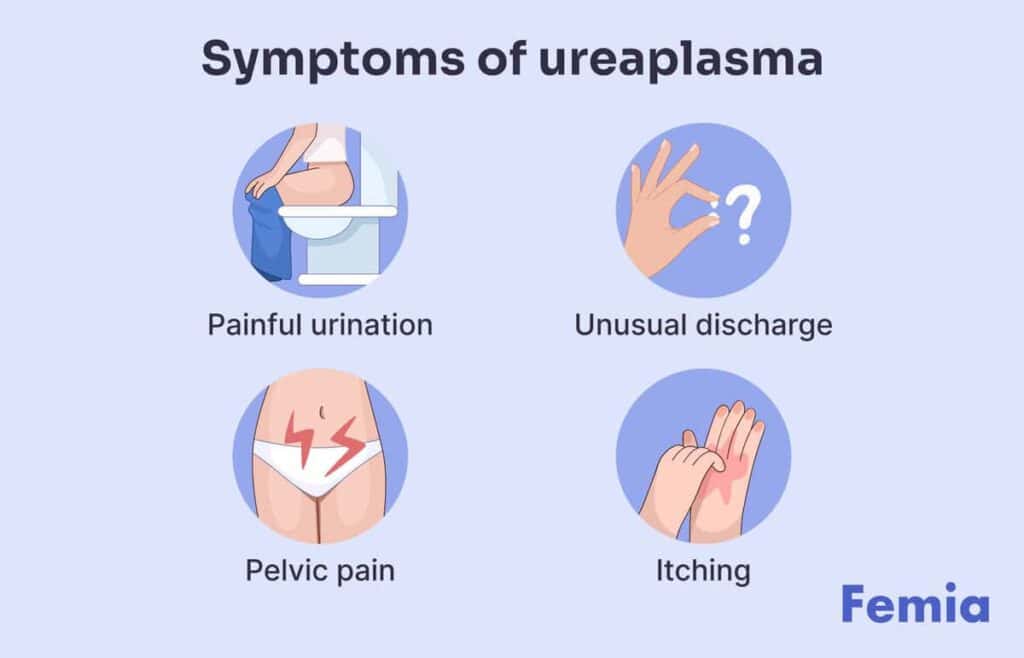
Symptoms of ureaplasma in females
Common ureaplasma symptoms can include:
- Painful urination. Pain and other discomfort felt while you pee might be signs of genital infection, including ureaplasma.
- Unusual vaginal discharge. Anaerobic bacteria, including ureaplasma urealyticum, are common causes of vaginal discharge in women, making up around 30% of all causes. It may also cause odor.
- Pelvic pain. Ureaplasma might sometimes lead to infection-induced pelvic inflammation and the development of endometriosis, which means that there might be some pelvic pain and discomfort.
- Itching or irritation. Like other genital bacteria, Ureaplasma can cause irritation, itching, and other discomfort around the genitals.
- Bacterial vaginosis. In some females, ureaplasma might cause bacterial vaginosis as the amount of lactobacilli drops and gets replaced by anaerobic bacteria.
- Belly pain. Ureaplasma might come with urethra inflammation and cause lower abdominal pain.
Ureaplasma symptoms in women can vary by type, severity, and duration. They can also overlap with other conditions in some women.
Important note: Ureaplasma does not always cause physical symptoms. Some women may experience this condition absolutely symptom-less, making it harder to detect the bacteria without testing.
How long can you have ureaplasma without knowing?
Ureaplasma species may exist in many women and cause no issues in their normal quantities and conditions. However, when the bacteria start growing, they might irritate tissue and cause infection.
Unfortunately, physical symptoms are not always present in women with ureaplasma. The infection can proceed asymptomatically for months and even years.
If you have mild symptoms or just suspect an infection, you may want to consider getting tested. And, if you want to prevent this condition from developing and running asymptomatically, you may want to have regular check-ups with your healthcare provider.
Diagnosis: Ureaplasma spp NAA
A nucleic acid amplification (NAA) test was designed to diagnose ureaplasma urealyticum infection. The test works based on the PCR amplification of the urease gene (UU1/UU2 Test).
During the test, healthcare providers collect urogenital swabs and extract DNA from them. A DNA fragment is then amplified by PCR to detect the infection.
The sensitivity and specificity of such tests are 100 and 98.9%.
Ureaplasma in pregnancy and newborns
The eight genera from the Mollicutes class (also referred to as mycoplasma) all play a significant role during conception and pregnancy.
Ureaplasma is no exception. By affecting the natural vaginal flora and causing other discomforting symptoms, ureaplasma is sometimes associated with adverse pregnancy effects. The sole presence of these bacteria is often insufficient to cause significant issues. However, an already-developed infection and its combination with other conditions (such as bacterial vaginosis or cervical incompetence) might induce preterm birth, low birth weight, and premature rupture of membranes. In some cases, ureaplasma may increase the risk of miscarriage.
In newborns, ureaplasma may result in congenital infections, such as meningitis and pneumonia, and respiratory issues like respiratory distress syndrome.
Given the potential implications caused by ureaplasma in pregnant females, early diagnosis and treatment are crucial. Luckily, NAA tests enable healthcare providers to detect the presence of these microorganisms in pregnant women and address them with relevant antimicrobial treatment. Timely treatment with pregnancy-safe antibiotics can effectively reduce adverse pregnancy outcomes.

If I have ureaplasma, does my partner?
Ureaplasma microorganisms are often part of a normal microbiome in healthy humans that helps digest food, fight infection, and retain reproductive system health. Nevertheless, ureaplasma is identified as an STI, meaning it can be transmitted during sex.
Ureaplasma can be spread by vaginal, penile, oral, or anal sexual contact. It can also be passed on via bodily fluids, such as saliva. Nevertheless, it’s more strongly associated with people who are not in a stable relationship—having more than one sexual partner within three months may increase the risk of acquiring ureaplasma.
Studies show that 7% to 63% of healthy men attending clinics had ureaplasma. This is only slightly lower than the number of women reported to have these microorganisms. Hence, the likelihood of transmitting the bacteria to your partner is rather high, though studies suggest that some men may develop adaptive immunity throughout their lifetime that can attenuate the symptoms of ureaplasma.
Due to the simple transmission of ureaplasma during sex, it’s important for both partners to get tested and receive effective treatment to prevent infection development.
How is ureaplasma treated?
If you suspect an infection or experience relevant symptoms, it’s recommended to see your doctor to receive timely treatment. After detecting the infection via ureaplasma spp NAA, healthcare providers typically prescribe antibiotic treatment. Antibiotic administration is shown to be effective in addressing intra-amniotic infections and inflammations, including ureaplasma. Common antibiotic types prescribed for this condition include:
- Doxycycline
- Azithromycin
- Erythromycin
If you are sexually active, it’s important that both you and your partner(s) get tested and receive treatment to prevent reinfection.
When it comes to ureaplasma in pregnant women, treatment also involves certain antibiotics that are safe for pregnant women, such as erythromycin. A doctor may also recommend regular monitoring and follow-up to ensure a healthy pregnancy.
How do you prevent ureaplasma?
Ureaplasma is common among sexually active adults and is diagnosed and treated rather easily. Still, there are a few simple tips to prevent infection and/or transmission:
- Consider using condoms or femidoms for all kinds of sexual intercourse, including vaginal, oral, and anal.
- Adhere to recommended storage and cleaning practices for sex toys.
- Consider getting regularly tested for ureaplasma and other STIs (especially if you have multiple sexual partners).
- If there are symptoms or suspicions of ureaplasma, consider getting tested together with your partner and receive the necessary treatment. If your partner has received treatment and you weren’t tested yet, consider abstaining from any form of sex until you get tested.
Questions from the Femia community
Can ureaplasma go away on its own?
Ureaplasma infections may go away on their own, but if it doesn’t, it can cause complications. A consultation with a doctor and a course of antibiotics is recommended to speed up the process, minimize health risks, and prevent reinfection and transmission.
Is ureaplasma always a sexually transmitted infection (STI)?
Ureaplasma is often identified as an STI, because it can be transmitted during sex. Still, it can be found in people who are not sexually active, which makes it different from other sexually transmitted infections.
Can ureaplasma affect fertility?
Yes. Ureaplasma can have a number of complications for your reproductive health, fertility, and pregnancy if the infection is left untreated.
Should I be worried if I have no symptoms?
Ureaplasma can often run symptom-free, which makes it hard to detect the infection without seeing a doctor. Even if you don’t notice any physical symptoms, it’s important to get tested and receive treatment if you suspect exposure to ureaplasma.
Can I get ureaplasma even if I wear a condom?
Condoms are proven to be 98% effective at preventing ureaplasma transmission if used right. Still, some creams and vaginal pessaries, such as thrush treatment, can reduce condoms’ efficiency and retain a risk of exposure.
Can an NNA test tell who gave me ureaplasma?
A ureaplasma spp NAA test is an effective method for detecting ureaplasma species and diagnosing an infection. However, the test can only indicate the presence of bacteria and not tell you when or how you acquired it.
The bottom line
As one of the most prevalent genital bacterium, ureaplasma is commonly found in females and males regardless of their sexual activity and can be easily transmitted to others during sex or via bodily fluid. It can present with a number of physical symptoms or none at all, which makes it crucial for you and any sexual partners to get tested and treated if you suspect exposure.
Now, you know more about the nature and symptoms of ureaplasma in females. Remember that just like any other infection, it can be addressed effectively via relevant treatment.
So, don’t overlook regular check-ups, and communicate openly with your healthcare provider to maintain your reproductive and overall health.
References
- Kallapur SG, Kramer BW, Jobe AH. “Ureaplasma and BPD.” Semin Perinatol, Apr. 2013. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3628630/
- Sung TJ. “Ureaplasma urealyticum or Ureaplasma parvum: what’s the difference?” Korean J Pediatr, Nov. 2013. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3859879/
- Kotrotsiou T, Exindari M, Diza E, Gioula G, Melidou A, Kaplanis K, Malisiovas N. “Prevalence and antimicrobial susceptibility of Ureaplasma urealyticum in asymptomatic women in Northern Greece.” Hippokratia, Oct. 2013. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4097411/
- Abou Chacra L, Fenollar F, Diop K. “Bacterial Vaginosis: What Do We Currently Know?” Front Cell Infect Microbiol, 18, Jan. 2022. https://pubmed.ncbi.nlm.nih.gov/35118003/
- Noh EJ, Kim DJ, Lee JY, Park JH, Kim JS, Han JW, Kim BC, Kim CJ, Lee SK. “Ureaplasma Urealyticum Infection Contributes to the Development of Pelvic Endometriosis Through Toll-Like Receptor 2.” Front Immunol, 4, Oct. 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6788432/
- Frølund M, Falk L, Ahrens P, Jensen JS. “Detection of ureaplasmas and bacterial vaginosis associated bacteria and their association with non-gonococcal urethritis in men.” PLoS One, 4, Apr. 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6448876/
- Biros E, Bodnár J, Biros I, Birosová E, Mojzis J, Hrivnák M, Klimcáková L, Findlay I, Mirossay A, Mirossay L. “Molecular detection of Ureaplasma urealyticum infection from clinical urogenital swabs.” Folia Microbiol (Praha), 2007. https://pubmed.ncbi.nlm.nih.gov/18062195/#:~:text=A%20simple%20nucleic%20acid%20amplification,fragment%20was%20amplified%20by%20PCR.
- Capoccia R, Greub G, Baud D. “Ureaplasma urealyticum, Mycoplasma hominis and adverse pregnancy outcomes.” Curr Opin Infect Dis. Jun. 2013. https://pubmed.ncbi.nlm.nih.gov/23587772/
- Bartkeviciene D, Opolskiene G, Bartkeviciute A, Arlauskiene A, Lauzikiene D, Zakareviciene J, Ramasauskaite D. “The impact of Ureaplasma infections on pregnancy complications.” Libyan J Med, Dec. 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7646542/#cit0009
- Tibaldi C, Cappello N, Latino MA, Masuelli G, Marini S, Benedetto C. “Vaginal and endocervical microorganisms in symptomatic and asymptomatic non-pregnant females: risk factors and rates of occurrence.” Clin Microbiol Infect. Jul. 2009. https://pubmed.ncbi.nlm.nih.gov/19558525/
- Taylor-Robinson D. “The male reservoir of Ureaplasma urealyticum.” Pediatr Infect Dis. Nov-Dec. 1986. https://pubmed.ncbi.nlm.nih.gov/3797322/#:~:text=Data%20from%2031%20different%20studies,nongonococcal%20urethritis%20were%20colonized%20likewise
- Catherine M. Wetmore, Lisa E. Manhart, M. Sylvan Lowens, Matthew R. Golden, Nicole L. Jensen, Sabina G. Astete, William L. H. Whittington, Patricia A. Totten. “Ureaplasma urealyticum Is Associated With Nongonococcal Urethritis Among Men With Fewer Lifetime Sexual Partners: A Case-Control Study.” The Journal of Infectious Diseases, Volume 204, Issue 8, 15, Oct. 2011. https://academic.oup.com/jid/article/204/8/1274/817358
- Oh KJ, Romero R, Park JY, Lee J, Conde-Agudelo A, Hong JS, Yoon BH. “Evidence that antibiotic administration is effective in the treatment of a subset of patients with intra-amniotic infection/inflammation presenting with cervical insufficiency.” Am J Obstet Gynecol, Aug. 2019. https://pubmed.ncbi.nlm.nih.gov/30928565/

Are baths safe during pregnancy? Learn about safe water temperatures and how you can enjoy a soothing, risk—free soak.
At 12 weeks pregnant, your baby’s organs are forming, and a bump may appear. Explore fetal development, symptoms, and what to expect in week 12.
Pregnancy brings a fresh and vibrant glow from within – but it doesn’t do much for your lips. Let’s check if you can get lip fillers while pregnant.